Paediatric Dietitians – referral criteria
Constipation is one of the commonest referrals into our outpatient service. Onset with weaning and potty training is common. Blood tests and imaging are not usually required. Faecal incontinence is commonly due to constipation with impaction and overflow diarrhoea. Contributing factors for constipation include pain, fever, inadequate fluid intake, reduced dietary fibre intake, toilet training issues, the effects of drugs such as sedating antihistamines or opiates, psychosocial issues, and a family history of constipation. Constipation is more common in children who are physically inactive or with impaired mobility or a neurodevelopmental disorder (e.g. cerebral palsy, Down’s syndrome or autistic spectrum disorder).
History
Two or more findings from below (also see key components table in NICE guidance https://
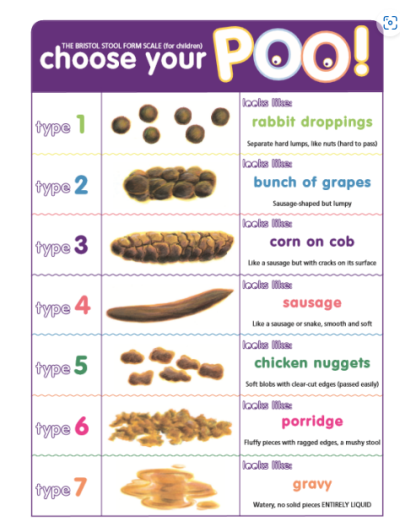
• Stool patterns – Fewer than three complete stools per week (type 3 or 4, see Bristol Stool Form Scale) (this does not apply to exclusively breastfed babies after 6 weeks of age); Hard large stool; ‘Rabbit droppings’ (type 1, see Bristol Stool Form Scale); overflow soiling (commonly very loose and smelly); large infrequent stools that can block the toilet
• Symptoms – Distress on stooling; Bleeding associated with hard stool; Straining; Poor appetite that improves with passage of large stool; Waxing and waning of abdominal pain with passage of stool; Evidence of retentive posturing: typical straight legged, tiptoed, back arching posture; Anal pain
• History – Previous episode(s) of constipation; Previous or current anal fissure; Painful bowel movements and bleeding associated with hard stoolsParents may confuse ‘straining’ with a child who is withholding stool.Typically the child with ‘overflow’ faecal incontinence due to constipation will pass small amounts of stool into their pants and seem unaware that they have done so. See constipation management below. Disimpaction is usually required before starting maintenance laxative.Bloody diarrhoea, faecal urgency or nocturnal diarrhoea suggests colitis. Refer these children to paediatrics.
Examination:
Plot height and weight in red book.
• The faecal mass of impaction can be difficult to palpate. Suspect faecal impaction if overflow soiling and/or faecal mass palpable abdominally
• Inspect anus to check normal anatomical placement or presence of anal fissures (digital rectal examination is not recommended in primary care).
• Inspect spine and check normal lower limb neurology.
Investigations:• No specific investigations (such as abdominal X-ray or ultrasound scan) are required in primary care to diagnose idiopathic constipation.• If the history-taking or physical examination shows evidence of faltering growth, treat for constipation and test for coeliac disease and hypothyroidism.• If constipation persists despite optimal laxative (macrogol) treatment for age consider performing Thyroid Function Tests and a coeliac screen.
We would like to see all these children in our clinics:
1. Early constipation in the first few weeks of life
2. Delayed passage of meconium > 48 hours
3. Family history of Hirschsprung’s Disease
4. Abdominal distension (not in keeping with age or excess weight) or vomiting (would need urgent review – call PAU mobile via switchboard to discuss emergency referral if obstruction thought likely)
5. Abnormal lower limb neurology or cutaneous lesion over spine suggesting spinal cord lesion
6. Ribbon stool pattern (more likely to indicate anal stenosis)7. Abnormal appearance of external genitalia or abnormal positioning of anus
8. Suspicion of child sexual abuse (based on knowledge of family background or other concerning behaviour)
Provide reassurance for the following infants who do not require referral or treatment
• Breast fed infants who only defaecate every few days but have no other symptoms of constipation or red flags.
• Do not treat infant dyschezia’ (characterised by at least 10 minutes of straining and crying before successful passage of soft stools in healthy infants aged under 6 months) with laxatives.
If the history-taking or physical examination shows evidence of possible child maltreatment, treat for constipation and refer to the NICE Pathway on child abuse and neglect.
If the physical examination shows evidence of perianal streptococcal infection, treat for constipation and also treat the infection.
Important things to discuss include:
1. Fluid intake – try to estimate how much, and what fluids the child is drinking.
2. Diet – it is important to discuss fibre, roughage and fruit/vegetable intake and provide signposting where needed (information in leaflet below).
3. Toileting routine – whether there is a routine of sitting on the toilet after meals, any particular anxieties around sitting on the toilet or defaecating. It helps if the child sits with their knees higher than their hips, so they may need a stool to support their feet. Many children are too scared to go for a poo at school and end up withholding.
4. Provide written information. The leaflet below provides helpful information https://
Medication:
Our usual treatment of constipation is movicol (or equivalent macrogol).
Assess for faecal impaction and treat with disimpaction regime if signs found or if bowels not opening for long periods of time with passage of large stools. There is a useful guide to disimpaction found here:
https://
Once disimpaction is completed, children will usually need to be on a maintenance dose for some time. Usual maintenance dose can be titrated to keep stools soft and easy to pass, but not liquid! Do not be scared to use maximal recommended dose for age and to restart treatment if problems reoccur.
Some parents find it tricky to get children to take movicol, especially in large doses – here are some tips to help:
1. Movicol does not need to be given all at once but can be split into smaller doses throughout the day
2. The granules can be mixed with something more palatable eg: yoghurt, mousse
3. Using a reward system eg: star chart or awarding ‘golden time’ can help with encouraging children to take regular medications.
4. Movicol can be made into ice pops or jelly. It can also be mixed into milkshakes (although you should mix the movicol with water first before adding to the milkshake).
If any child has any of the ‘red flags’ or symptoms persist despite optimal treatment, please consider referring to Children’s Outpatients for further investigation.
Please call the on-call paediatric assessment unit phone (PAU) via switchboard if history or examination raises a concern about possible abdominal obstruction.
Discussion of cases where need for referral, or degree of urgency, is uncertain is encouraged through Advice & Guidance on ERS.
We have a nurse led (PACE) clinic service who can support children and their families to treat constipation. All children are seen by a Paediatric Consultant first to exclude significant pathology before being referred to PACE.
The school nursing service (depending on borough of child and whether they are in a specialist educational setting) may be helpful in supporting children with behavioural causes of stool withholding and encopresis (passing stool in inappropriate places).
Supporting information:
https:/