Paediatric Dietitians – referral criteria
This does not cover the acute management of asthma. For acute management, see PAU – wheeze in children.
This is intended to be a guide for managing chronic asthma in children over 5 years of age.
Diagnosis of asthma in children is clinical and based on the BTS/Sign guidelines 2019 which states that factors involved in a clinical assessment include:
Episodic symptoms
- More than one of the symptoms of wheeze, breathlessness, chest tightness and cough occurring in episodes with periods of no (or minimal) symptoms between episodes. Note that this excludes cough as an isolated symptom in children.
- For example:
- a documented history of acute attacks of wheeze, triggered by viral infection or allergen exposure with symptomatic and objective improvement with time and/or treatment
- recurrent intermittent episodes of symptoms triggered by allergen exposure as well as viral infections and exacerbated by exercise and cold air, and emotion or laughter in children.
- An historical record of significantly lower FEV₁ or PEF during symptomatic episodes compared with asymptomatic periods provides objective confirmation of the obstructive nature of the episodic symptoms.
Wheeze confirmed by a healthcare professional on auscultation
- It is important to distinguish wheezing from other respiratory noises, such as stridor or ‘rattly’ breathing.
- Repeatedly normal examination of chest when symptomatic reduces the probability of asthma.
Evidence of diurnal variability
- Symptoms which are worse at night or in the early morning.
Atopic history
- Personal history of an atopic disorder (ie eczema or allergic rhinitis) or a family history of asthma and/or atopic disorders, potentially corroborated by a previous record of raised allergen-specific IgE levels, positive skin-prick tests to aeroallergens or blood eosinophilia.
Absence of symptoms, signs or clinical history to suggest alternative diagnoses
Children with a high probability of asthma based on clinical assessment, should be commenced on a 6 week course of standard asthma treatment, which is usually an inhaled corticosteroid with salbutamol as a reliever. There should be a review in place at 6-8 weeks which should assess response, using PEFR as an objective measure if the child is able and old enough. If there is little, or no response, consider:
- The possibility of alternative diagnoses
- Medication technique and compliance
- Psychosocial factors
- Whether they need a paediatric opinion (see under ‘Referral Information’)
If there is a good response to initial treatment, please titrate inhaled corticosteroids to the lowest dose which controls symptoms, and ensure that good education has taken place. This should include a written ‘Allergy Action Plan’, and a plan for regular medical review. Discuss avoidance of possible triggers such as domiciliary cigarette and other smoke.
Reviews
For children with an established diagnosis of asthma, who are undergoing community review it is important to consider:
Symptom Control
- What is the use of reliever (usually salbutamol) therapy? How frequently is it required?
- Are there interval symptoms – nocturnal cough or exercise induced cough/wheeze?
- Have they needed oral steroids for an acute attack, either in primary or secondary care?
- Have they needed emergency care (may not necessarily result in treatment with steroids)
- Has the child completed the ‘Asthma Control Test’ specific to their age group? A link can be found in ‘Supporting Information’.
- What is their compliance with medication like (both self-reported and objectively from practice records)?
Objective measures
- What is their height and weight, as plotted on an appropriate age-specific centile chart?
- What is the PEFR and is this appropriate for age/height?
- How many prescriptions have been filled for preventers (usually salbutamol from the practice)?
Social issues
- Are there smokers in the family? Has smoking cessation advice been discussed?
- Are there pets at home – has the possibility of allergy been discussed?
- Is there a possible issue with house dust mite? Has reduction of dust mite exposure been broached?
- Is this seasonal – either related to Autumn/winter viruses or pollen in summer?
- Is this affecting education? What time have they had off school due to health?
- Consider compliance with medication/inhaler technique (see under management)
- Do the family know the advice for action in an acute attack – do they have a written ‘Asthma Action’ plan?
Every medical encounter is an opportunity to educate children and parents/carers about their asthma. This should involve:
- Discussing emergency regimes/treatment, including when and how to seek urgent medical help
- Medication – compliance with prescribed medications and inhaler technique
- Providing or reviewing a written ‘asthma action’ plan
- Discussing any triggers or exacerbating factors
- Eliciting any psychosocial factors which may have an impact, including family support, mental health, any safeguarding concerns.
Children who have the following ‘Red Flags’ should be referred for advice:
- Faltering growth
- Unexplained clinical findings (e.g. focal signs, abnormal voice or cry, dysphagia, inspiratory stridor)
- Symptoms present from birth or perinatal lung problem
- Excessive vomiting or posseting
- Severe upper respiratory tract infection
- Persistent wet or productive cough
- Family history of unusual chest disease
- Nasal polyps
Children who have had the following ‘additional considerations’ should also be sent for Paediatric Assessment via outpatient clinic:
- Diagnosis unclear or in question
- Child is on regular low dose ICS plus either LABA or LTRA and symptoms not well controlled
- Poor response to monitored initiation of asthma treatment
- Severe/life-threatening asthma attack
- Patient or parental anxiety and need for reassurance
Please note that this does not cover the action to be taken in an acute asthma attack. This is for the management of chronic asthma in children.
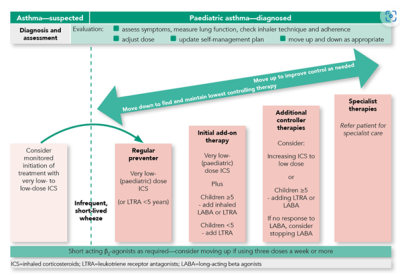
Please see below the algorithm for the management of paediatric asthma. Full details can be found on the SIGN website.
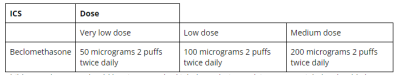
The following table shows the dose of standard non-proprietary beclomethasone inhaler dose:
Children and parents should be given standard inhaler technique advice. An MDI inhaler should always be given via a spacer in children. In young children (< 6 years), the spacer should come with a mask and it is important to check that this fits snugly over nose and mouth. In older children, a spacer with a mouthpiece is recommended but it is important to check that they can manage a good seal with their lips around the mouthpiece.
The spacer should be cleaned monthly by washing in hot water and washing up liquid. They should be advised to leave it to air dry (rather than rubbing with a tea towel which creates static and reduces drug delivery to the lungs). They will need to be changed for a new spacer every 6-12 months.
Children on regular inhaled corticosteroids should be advised to brush their teeth and rinse their mouth after taking the medication.
https://
https://
Peak flow (PEFR) is difficult to do reliably in young children. From the age of 6 years, children can start to practice performing a peak flow as part of their standard asthma reviews. This should be plotted on a normogram for height and age. Initial attempts are likely to be inaccurate, as it takes practice to develop a good technique. The below is a video for parents on how to perform peak flow.
https://
Children should have their height and weight plotted in the Red Book or appropriate age-specific centile chart.
A child who is obese according to a centile BMI chart, should be referred for dietary advice and intervention. Education regarding healthy diet and weight maintenance should be offered to all children and families.
Smoking cessation advice and available resources should be offered to Young People and parents who smoke.
Once control has been achieved, it is important to maintain children on the lowest possible dose of inhaled corticosteroids – this should be reviewed every 3 months with a view to reducing steroids, where possible by 25-50% of starting dose.
There may be co-existing rhinitis which can be treated with intra nasal steroids as a first line therapy.
Always be mindful of any safeguarding or psychosocial factors. Reviews of childhood asthma deaths suggest that children who have multiple missed appointments, poor medication compliance, high SABA use and a previous life-threatening asthma presentation are at higher risk of a further life threatening presentation.
For Children with any ‘red flags’ or ‘additional considerations’ should be referred to Paediatric Outpatients via ERS, with as much supporting information as possible.
Children who are on regular very low dose ICS plus either a LABA or LTRA and have not achieved adequate control of symptoms should also be sent for Paediatric Assessment in outpatients via ERS.
It is important that children bring their current inhalers and spacer devices with them to the appointment. This is so we can check inhaler technique as part of the appointment. It is also important for parents to bring their copy of the ‘asthma action’ plan.
If you are unsure, we are happy to discuss the child with you – if the child is known to a Consultant here, you can ask them to call you back by leaving a message with the Paediatric Admin Office. If they are not known to us yet, please ask for advice via Advice & Guidance on ERS or the Paediatric Advice Telephone.
For the full BTS/Sign guideline, please click on link below
We have a parent information leaflet on recognising the signs of an asthma attack which can be found here:
NEED ASTHMA LEAFLET HERE
All children should have a written ‘asthma action’ plan. This is the one we recommend:
https://
Here is some additional information about spacer use and care from Asthma UK:
https://
The Asthma Control Test for 4-11 year olds can be found here:
https://