Paediatric Dietitians – referral criteria
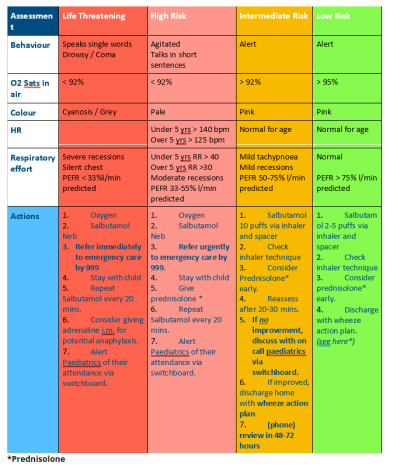
A clinical assessment will help to assess the urgency of the child’s condition. Oxygen saturations in young children should only be measured if a paediatric saturation probe is available.
An attempt to measure peak expiratory flow should be made in all children aged 6 years and over. The normal values can be found here:
http://
A guide on how to perform peak expiratory flow can be found here:
https://
- Try to avoid in < 2 years old and episodic wheeze, i.e. distinct episodes of wheeze with upper respiratory tract infections only; especially if there is no history of interval symptoms and no other triggers.
- Give prednisolone 1mg/kg (max 40mg) as early as possible in multi trigger wheeze / asthma or if there is a history of atopy or family history of asthma/atopy. A standard course is 3 days. If still significant symptoms after 3 days, further steroids and review in secondary care paediatrics should be considered.
Please consider whether an alternative diagnosis is likely, such as:
- Chest infection – high fevers, wet cough, focal signs on chest auscultation
- Foreign body aspiration – usually from history, focal chest signs
- Croup – inspiratory stridor, sudden onset
- Bronchiolitis in < 12 months old – especially if widespread wheeze and crackles
Things to consider at phone/in person review:
Following an acute attack:
- Check if improving – if child is unable to progress through the salbutamol weaning plan, or has deteriorated/’gone backwards’, please refer to Paediatrics for same day assessment.
- Check need for further steroids
- Review triggers leading to attack i.e. (allergens / compliance with meds / anxiety / weather/ exercise or exertion)
- Check need for preventer inhaler – interval symptoms between attacks / use of Salbutamol > 2 – 3 times per week or > 2 attacks per year (see ‘chronic asthma’)
- Check the child has sufficient salbutamol and an appropriate spacer available for future episodes
- Check inhaler technique.
Ongoing management
- If using short acting B2 agonist more than three times a week consider regular preventer therapy- In the under 5 age group this can be either an inhaled low dose corticosteroid or leukotriene receptor antagonist (Montelukast)
- Consider referral to Paediatrics if the child has required an inpatient admission or there are recurrent episodes over a several month period. Similarly, also consider referral if concerns over compliance with treatment or parental anxiety.
Here are some useful videos to guide parents:
https://
https://
- Check wheeze action plan in place
This is the one we recommend:
https://
- Check if any ‘Red Flags’ are present which would trigger a referral to Paediatric Outpatients.
If a child presents to primary care for 48 hour review but has deteriorated, or is unable to progress through the salbutamol weaning plan, please refer to Paediatrics for same day assessment via switchboard.
The following are considered ‘Red Flags’ for significant respiratory disease and referral to Paediatrics is recommended. If you are unsure of the need or of the level of urgency, please discuss via the on call telephone (if child is acutely unwell) or via Kinesis.
- Failure to thrive
- Focal signs
- Abnormal voice /cry
- Dysphagia
- Inspiratory stridor
- Symptoms present from birth / perinatal lung problems
- Excessive vomiting
- Persistent wet cough
- Family history of unusual chest disease
- Nasal polyps
- Parental anxiety / need for reassurance
- Diagnosis unclear
For children with acute wheeze who are identified as life threatening or high risk in primary care, please arrange paramedic transport to hospital via 999. It is helpful to let on call paediatrics know to expect them by calling us via switchboard.
For children who are in the intermediate risk category but not improving, please refer to on call paediatrics via switchboard. We may ask them to come to A&E rather than PAU if they sound unwell, as we have easier access to resuscitation facilities there, but they will still be seen by the paediatric team.
If a child is well enough to go home with safety netting advice, please consider whether they need outpatient Paediatric input. Children in the following categories are considered higher risk for a future life threatening episode:
- Having had 1 or more life threatening asthma attack(s).
- More than 2 steroid courses in last 12 months.
- More than 2 hospital admissions for wheeze in the last 12 months.
- Healthcare worker or parental concern of asthma control.
- Exposure to environmental tobacco smoke
- Younger age
- Obesity
- Co-morbid atopic conditions triggering wheeze
For the full BTS/Sign guideline, please click on link below
All children should have a written ‘asthma action’ plan. This is the one we recommend:
https://
Here is some additional information about spacer use and care from Asthma UK:
https://
The Asthma Control Test for 4-11 year olds can be found here:
https://