Neurodiversity information for parents and young people
Read this information alongside your child’s copy of ‘My personal asthma plan’. (Your GP or other healthcare professional will complete your child’s personal asthma plan in discussion with you.)
Your child’s salbutamol (reliever) inhaler
Everyday management of your child’s asthma probably includes a salbutamol blue (reliever) inhaler like the one in the picture. Brand names for this include Ventolin, Airomir, Asmalal, Easyhaler, Pulvinal, Salamol, Easi-Breathe, Salbulin.
When your child uses their reliever inhaler, make sure they use it with a spacer (see photo). Using a spacer makes the salbutamol dose much more effective. This applies to children of all ages.

Your child’s need for the reliever inhaler is probably now reducing.
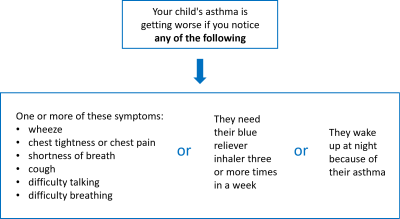
The following gives guidance on signs to look out for.
This will help you recognise when your child’s symptoms are getting worse, or when they are experiencing an asthma attack.
Signs that your child’s asthma is getting worse
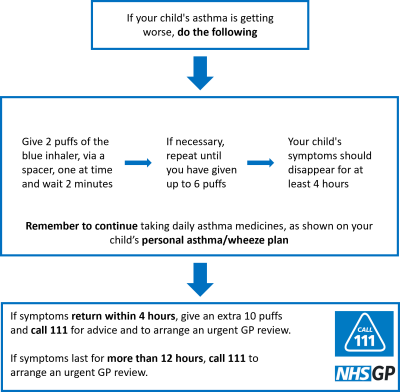
What to do if your child's asthma is getting worse
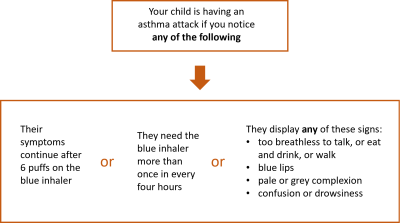
Signs that your child is having an asthma attack
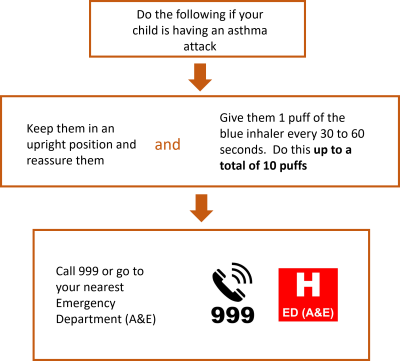
What to do if your child is having an asthma attack
Do the following after every asthma event, including mild symptoms or full attack
| Within 2 working days of the asthma attack, contact your GP to arrange a post attack review for your child.During this review, your GP or asthma nurse will check on your child’s recovery. |
| Within 4 weeks after the asthma attack, arrange a full follow up review with your GP or at the Kingston Hospital Children’s Outpatient Department. |
Important information
![]()
Take your child to your nearest Emergency Department (A&E) immediately if they need to use their reliever (salbutamol) inhaler more frequently than every 4 hours.
More information
For Asthma and Lung UK information about asthma
For Asthma and Lung UK information about using an inhaler
For Allergy UK advice on asthma
For videos of signs of increased work of breathing including grunting and abdominal breathing
For Kick-it Stop Smoking Service advice on giving up smoking
Contact information
Paediatric Admin Team, Monday to Friday 9 am to 5 pm