Neurodiversity information for parents and young people
Before using insulin
Before using insulin, we recommend you test your blood glucose levels.
The frequency of your tests will depend on your level of blood glucose control.
Your nurse or doctor can advise you on this. Speak to them about the glucose “target levels” that you aim to achieve with your new treatment.

Make a note of your target glucose levels.
Glucose is a sugar carried in the bloodstream that your body uses for energy. If you have diabetes, your blood glucose levels can be erratic and sometimes they become extremely low.
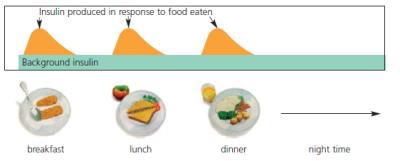
People who do not have diabetes produce a constant level of insulin. This is called 'background' insulin. When they eat, their bodies produce more insulin to reduce the glucose in the food they have just eaten.
If you have diabetes your may not produce enough (or any) insulin or your body cannot use your insulin properly. This causes a rise in your blood glucose levels.
Injecting insulin reduces your blood glucose levels to more normal levels.
Different types of insulin
Different types of insulin work in slightly different ways. They may need to be taken at specific times, such as before eating.
Your nurse or doctor will discuss with you when you need to take your insulin and why.
- Long acting insulin: Background insulin that lasts for up to 24 hours.
- Quick acting insulin: Meal time insulin that works quickly and usually for 3 to 5 hours.
- Premixed insulin: A mix of insulins usually given daily or twice daily to provide background and meal time insulin requirements.
Food storage
Follow this guidance when you store your insulin.
- Keep insulin stored in a fridge at 2 to 8 degrees centigrade.
- Do not store insulin near the fridge cooling element. If your insulin freezes, we have to destroy it.
- Once you are using your loaded pen you can store it at room temperature.
- On extremely hot days, keep it in an insulated bag or in the fridge (away from sunlight and high temperatures).
Check your insulin before you use it
Follow this guidance before you use your insulin.
- Check the label to make sure it is still the right type of insulin for you.
- Make sure the insulin is not past the expiry date.
- Do not use it if the protective cap is missing or loose.
- Do use it if it has not been stored properly or has frozen.
- Do not use it if it is not uniformly cloudy and white when you mix it up.
How often will I need to inject my insulin?
Everyone’s routine is different. You may inject your insulin between 1 to 5 times a day. It depends on which routine best suits your lifestyle and diabetes.
Your doctor or diabetes nurse will discuss this in more detail when you start insulin.
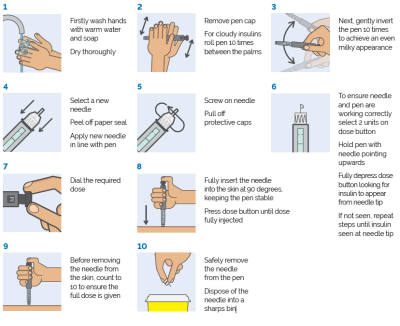
How do I inject my insulin?
Your nurse or healthcare professional will show you how to inject your insulin. They will advise you on how many units of insulin to inject when you first start insulin. This will be your starting dose and it may increase, depending on your blood glucose levels.
- You need to inject your insulin under your skin into your fatty tissue.
- If you inject your insulin into a muscle, this will affect its absorption and may cause erratic blood glucose levels.
- Always vary the sites where you inject. This will avoid lumps developing which will affect your blood glucose control.

Always record your blood glucose level and tell your diabetes nurse who will advise you on how to adjust your insulin dose.
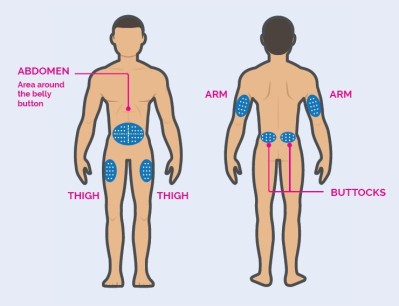
Insulin injection sites
Your diabetes nurse may advise you to inject your insulin into a particular site at different times of day.
Always choose different areas to inject into to avoid lumps or swellings from repeatedly injecting into the same place.
Insulin injection technique
Sharps disposal
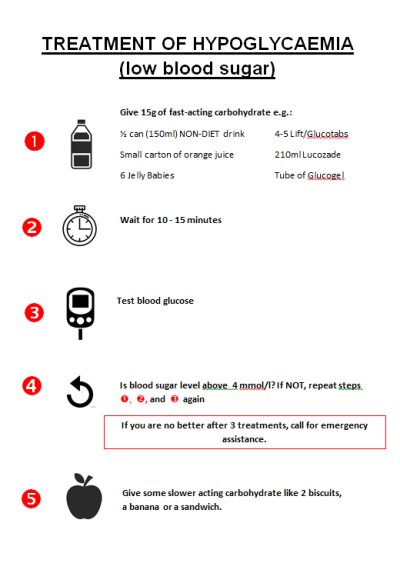
Hypo means your blood glucose levels drop below 4 mmol/L.
Symptoms of a hypo vary from person to person, but you will feel 'different' quickly.
Early symptoms of a hypo include the following:
- sweating heavily
- feeling anxious
- trembling and shaking
- tingling lips
- hunger
- going pale
- palpitations (erratic heartbeat).
If you miss these early symptoms, they may get worse and include the following:
- slurring your words
- behaving oddly
- being unusually aggressive or tearful
- having difficulty concentrating.

Treat your hypo as soon as possible. If you do not treat your hypo, you may become unconscious.
Insulin side effects and allergy
Insulin side effects are rare, but they can include the following:
- Stinging around the injection site (usually temporary).
- If you inject into the same site, you may develop fatty lumps or atrophy (tissue wastage). You can avoid this by regularly changing the site where you inject.
![]()
Contact your diabetes nurse or GP if you experience hard lumps or skin pitting on your injection sites.
Insulin allergy is extremely rare, but it can include the following:
- A temporary change in vision. This can be due to your changing blood glucose levels.
- Painful neuropathy (nerve damage). This can be due to a rapid improvement in your blood glucose levels.
Emotional support
Diabetes can have an emotional impact as well as a physical one. This is especially true when you start insulin.
You may need support from family, friends or healthcare professionals.
Ask your diabetes team about a talking therapies service called Richmond Wellbeing or use this link:
- Richmond Wellbeing Service. This offers free talking therapy to help you feel better.
Feeling unwell
If you have Type 1 or Type 2 diabetes, any illness or infection can cause your blood glucose levels to rise. This may happen even if you are not eating regularly.
This sudden rise in blood glucose may be the first sign of underlying infection or virus.
- Keep taking your insulin even if you are not eating.
- If you do not feel like eating, try some light, easily digestible foods such as soups and milky puddings.
- Ensure you drink plenty of sugar free fluids or water to prevent dehydration. This is especially important if you have Type 1 diabetes.
- Test your blood glucose levels more frequently. Test them at least four times per day.
- Report your blood glucose readings to your GP or diabetes team. They may advise you to increase your insulin or other medicines.
- We recommend that people with diabetes have regular flu and pneumococcal vaccinations. Speak to your diabetes team for more information.
![]()
Make a GP appointment if you think you may have an infection which requires antibiotic treatment.
If your blood glucose levels are on the low side because your appetite is down, you may need to reduce your medication and/or insulin. Speak to your GP or diabetes team for advice.
Ketones
- If you have Type 1 diabetes your body may produce ketones (acids) when you are unwell. If ketones are left untreated they may cause diabetic ketoacidosis which requires urgent medical treatment.
- Speak to your diabetes team about testing you for the presence of ketones.
Employment
Tell people at work
If you inject insulin and monitor your blood glucose levels, you will know these are things you need to do to keep safe.
Do not feel embarrassed about it. Talk to your colleagues about it.
If you are at risk of hypos, tell your colleagues how to spot your symptoms and how to help you if you experience a hypo. This will make sure you get the right kind of help and prevent your colleagues from panicking.
Talk to your employment first aider so they know how to act in an emergency.
Hypo at work
If you have a hypo at work, talk to your colleagues afterwards. Explain to them why it might have happened. Let them know it can happen if diabetes is treated with insulin or certain diabetes medication.
Rights at work
If you live in England, Scotland or Wales, your rights at work (as a diabetic) are set out in the Equality Act 2010. Your employer may need to make ‘reasonable adjustments’ so you can do your job.
For example, if you have diabetes and you need to eat at set times to stay on top of your blood sugar levels, you may not be able to shift lunch rotas easily. A reasonable adjustment could be for your employer to allow you to have your lunch break at the same time every day.
You will need regular check ups as part of your 15 Healthcare Essentials. Make sure your line manager understands why these checks are necessary. You do not need to apologise for them.
It can be daunting when you start insulin, especially if you need several injections every day.
Some people find it useful to have time off while they establish their new routine.
Discuss this with your GP. They may be able to request some time off if this is appropriate for you.
Insulin Passport
If you use insulin for your diabetes, you can choose to carry a credit card sized paper record called the Insulin Passport.
This can record:
- Up to date details of the type of insulin, syringes and pens that you use.
- Emergency information that tells people what to do if they find you ill or unconscious.
- Other information to help in an emergency, including contact names and telephone numbers and other medication that you may need.
Speak to your diabetes team about applying for an Insulin Passport.
You can still drink, but you need to be aware of how it can affect your body and how to manage this effect.
Alcohol can cause hypoglycaemia (a hypo) shortly after drinking. This effect can last for up to 24 hours after drinking.
![]()
If you drink alcohol, you should check your blood sugar before you go to bed.
If your blood sugar is lower than 8mmol/L we advise you to have a snack before bed. This will help you to avoid a low blood sugar reaction while you sleep.
The symptoms of too much alcohol and hypoglycemia can be similar (sleepiness, dizziness and disorientation).
It is a good idea to wear an ID that says 'I have diabetes'. This will stop people confusing your hypo symptoms with drunkenness.
Speak to your diabetes team about your drinking habits and how best to manage your insulin when you drink.
Food
Follow the healthy eating guidelines below. They will help you to control the glucose and fat levels in your blood and manage your blood pressure.
- try to eat a variety of foods
- eat three regular meals a day
- include starchy carbohydrates
- eat foods which are high in fibre
- reduce your intake of foods and drinks with a high sugar content
- avoid special diabetic foods
- cut down on the amount of fat in your diet
- choose a healthier type of fat
- try to achieve and maintain a healthy weight for your height
- try to use less salt and salty foods
- drink alcohol in moderation only.
Exercise
If you take insulin, physical exercise will be beneficial for your physical and mental wellbeing.
It may have an effect on your blood glucose levels. You may need to adjust your insulin doses or have a snack before you exercise.
Talk to your diabetes team if you are unsure how your body may respond, or if you belong to one of the categories listed below.
- You are above 35 years old
- You have had diabetes for more than 10 years
- You have high blood pressure, high cholesterol, or a family history of heart problems
- You smoke
- You have had diabetes related complications that have affected your eyes, kidneys, nervous system or large blood vessels.
![]()
Delay or avoid exercise if you have high blood glucose levels of 15mmol/L or more and ketones in your urine or blood.
Vigorous activity will increase your blood glucose levels and ketone levels further. Speak to your diabetes team for advice on how or when to exercise safely.
Runsweet offers information on safe exercise for runners with diabetes
Taking insulin need not affect your ability to travel abroad, but you need to plan ahead.
- Carry a spare insulin pen and other equipment (needles, testing strips, etc) in case you need them.
- Carry your diabetes equipment in your hand luggage, not in your main luggage.
- “In use” pens can be kept at room temperature. If you are going to a hot climate or taking a long, hot journey, we advise you to keep your insulin in a cool bag.
- Do not allow your insulin to freeze.
- If you are carrying insulin, we advise you to carry your diabetes ID and a letter from your nurse or doctor.
- Plan ahead for travel between time zones. Ask your diabetes team for advice if you need it.
- Make sure your travel insurance covers your existing medical conditions and any diabetes related emergency that may occur.
Insulin and the DVLA
Tell the DVLA if:
- your insulin treatment lasts (or will last) over 3 months
- you had gestational diabetes (diabetes associated with pregnancy) and your insulin treatment lasts over 3 months after the birth
- Yyou get disabling hypoglycaemia (low blood sugar) or a medical professional has told you that you are at risk of developing it.
The DVLA will send you a detailed letter explaining licensing requirements and driving responsibilities.
The rules are different depending on what vehicle you want to drive: Class 1 (car or motorbike) or Class 2 (lorry or larger vehicle).
Glucose testing requirements when you drive
You must test your blood glucose levels every time your drive. Test your levels no more than 2 hours before the start of your first journey and every 2 hours while you drive.
If your test indicates your glucose is 5.0mmol/L or less, eat a snack.
Do not drive if your test indicates your glucose is less than 4.0mmol/L or you feel 'hypo'.
Real time or flash glucose monitoring
If you use a real time (RT-CGM) or flash glucose monitoring (FGM) to check your glucose levels and your reading is 4.0mmol/L or below, you must stop driving. Confirm your level with a finger prick glucose test.
Your finger prick glucose level must be at least 5.0mmol/L before you start driving.
Appropriate glucose monitoring systems
Group 1 drivers may now use finger prick glucose testing and continuous glucose monitoring systems (FGM and RT-CGM) for the purposes of driving.
Group 2 drivers must continue to use finger prick testing for the purposes of driving. RT-CGM and flash glucose monitoring systems are not legally permitted for the purposes of Group 2 driving.
All glucose monitoring systems used for the purposes of Group 1 driving must carry the CE mark.
As there are times when FGM and RT-CGM users are required to check their finger prick glucose, users of these systems must also have finger prick glucose monitors
There are different requirements for group 1 and group 2 drivers. Further information can be found on the DVLA website (see link below).
Glucose monitoring methods
Group 1 drivers may now use finger prick glucose testing and continuous glucose monitoring systems (FGM and RT-CGM) for the purposes of driving.
These glucose monitoring systems must carry the CE mark.
Group 2 drivers must continue to use finger prick testing for the purposes of driving.
It is illegal for a Group 2 driver to use RT-CGM and flash glucose monitoring systems for glucose testing when driving.
Users of FGM and RT-CGM users must also have finger prick glucose monitors available. This is for use when they are required to check their finger prick glucose.
For further information go to the DVLA website.
Developing a hypo while driving
If you develop a hypo while you drive, stop your vehicle safely as soon as possible.
Switch off the engine, remove the keys from the ignition and move from the driver’s seat.
Do not start driving again until 45 minutes after your finger prick glucose has returned to normal. Normal means at least 5.0mmol/L.
Useful websites
Contact information
Diabetes Specialist Team
Teddington Memorial Hospital
Hampton Road
Teddington
TW11 0JL