Neurodiversity information for parents and young people
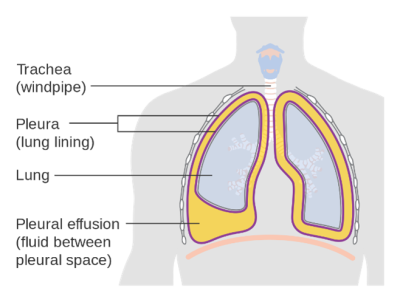
A pleural effusion is when fluid develops between the two layers of tissue (known as the 'pleura') that surround the lung. If the effusion is large, it can put pressure on the lung. This can lead to difficulty in breathing, cough and sometimes pain.
Pleural effusions can occur around one lung (unilateral) or both lungs (bilateral).
Causes
There are many causes of pleural effusions. The causes tend to be different if the effusion is unilateral or bilateral.
- Unilateral pleural effusion is commonly caused by a problem within the lung itself, such as infection, inflammation or cancer.
- Bilateral pleural effusion is commonly caused when the heart, liver or kidneys are not working normally. Bilateral effusions often improve with treatment of the underlying cause.
Pleural aspiration and drainage
Pleural aspiration and pleural drainage are done to diagnose a problem. They are similar procedures. But drainage involves an additional step to allow more fluid to be removed. You will be told whether you are having an aspiration or drainage before the procedure.
Pleural aspiration
For an aspiration, local anaesthetic will be used to numb your skin. A small needle is then passed into your chest to remove a sample of fluid. The procedure often takes about 30 minutes.
Pleural drainage
For a drainage, local anaesthetic will be used to numb your skin. A small plastic tube is then passed into your chest and connected to a drainage bag. This allows a large amount of fluid to be removed.
The chest tube is then removed and a dressing is applied. Pleural drainage usually takes about 45 minutes.
Depending upon the cause of the effusion you may need other treatments to stop the effusion returning. This can also include further pleural drainage.
Advantages
A pleural aspiration allows a small amount of fluid (20 to 100mls) to be sent for tests. This is used to help work out what caused the effusion. This will also help us to understand if the fluid is likely to return.
Pleural drainage allows fluid to be sent for tests and also allows fluid (up to 1500mls) to be removed to help improve your breathing.
Risks
Pleural aspiration and drainage are generally considered very safe procedures. However, as with all medical procedures, there are risks.
These include:
- Bleeding
The risk of serious bleeding is low.
We minimise this through:- asking you to have blood tests before
- stopping certain medications
- using an ultrasound machine to locate the fluid.
- Infection
We use anti-septic techniques to try to minimise the risk of infection.
- Air into the pleural cavity (pneumothorax)
The risk of this is low. If a small amount of air enters the pleural cavity you may need to return to the Medical Day Unit after 1 to 2 days to have a repeat chest X-ray. If a large amount of air is present, you may need to be admitted to the hospital and have a chest tube inserted.
- Internal organ injury
There is a small risk of injury to the lung or other internal organs, including the heart, liver, and spleen. This risk of this is reduced using ultrasound.
- Pain
The local anaesthetic can sting, and you might feel a ‘catch’ as the needle enters the pleura. However, this will last less than one minute, and most people do not find the procedure very painful.
Before the procedure
- You will need to have a blood test to check that your blood clots normally. This will usually be completed before the day of the procedure.
- Some medications may need to be stopped because they increase the risk of bleeding - for example aspirin, clopidogrel, heparin, apixaban, rivaroxaban, dabigatran and warfarin.
Tell the doctor
Tell the doctor if you are taking any of these medications as soon as possible. You may need to stop taking them before the procedure.
On the day
On the day of the drainage or aspiration:
- you can eat and drink as normal and take all your regular medications (unless you have been advised by your doctor to stop any)
- come to the Medical Day Unit, which is on the 7th Floor Esher Wing (see map)
- the procedure will be explained to you, and you will be asked to sign a consent form
- the doctor will use cold gel and an ultrasound machine to mark a site to remove the fluid
- the doctor will then confirm if you are having a pleural aspiration or drainage.
Alternatives
A pleural aspiration gives your doctor very specific information about the nature of the fluid and what may have caused it. If you decide not to have a pleural aspiration, the effusion can be monitored using chest X-rays and CT scans. However, without an aspiration the cause may not be known.
In some cases, your doctor may instead recommend you have a more invasive procedure using keyhole surgery.
![]()
After the procedure
A small dressing will be applied afterwards. You can remove this after 24 hours.
You do not need to be escorted home. Most people feel well enough to return to their usual activities by the following day.
The results of the pleural aspiration may not be available for several days. The results will be available to the doctor who asked you to have the pleural aspiration. They will usually contact you and your GP with the results. If you are under the Respiratory clinic, the results may be discussed with you at your next appointment.
If you have discomfort after the procedure, it is safe to take a simple pain killer, such as paracetamol, as long as you have not been asked to avoid this.
![]()
- Medical Day Unit (between 9am to 4pm)
- Emergency Department (A&E) at other times.
The Medical Day Unit is on the 7th Floor, Esher Wing.
Contact information
Respiratory department
Telephone:
020 8934 2321, option 3