Neurodiversity information for parents and young people
Here we offer advice on plantar fasciitis. We explain what it is, how we manage it, the treatment we may offer you, and the different options that are available to you.
About plantar fasciitis
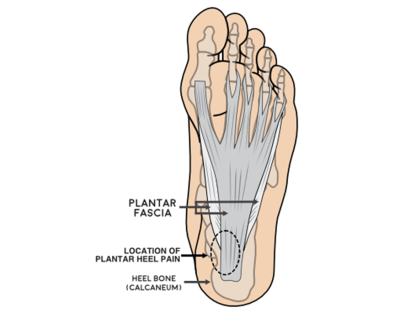
Plantar fasciitis is the development of inflammation in the plantar fascia in your foot.
Plantar fasciitis is the most common cause of foot pain. The pain typically occurs in the heel of the foot and can be quite painful.
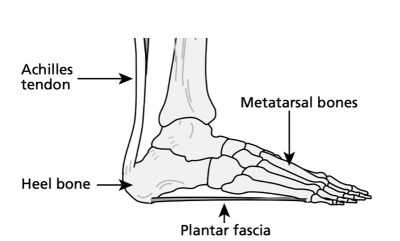
Plantar fasciitis occurs when your fascia is overused or over stretched. This causes inflammation, most commonly to the area where the fascia attaches to your heel bone.
This inflammation makes it painful to walk, stand for long durations and use your foot for everyday activities. Most people experience pain in one foot or another, but it can often occur in both feet at once.
Symptoms
- heel pain
- pain in the arch of the foot
- stiffness in the sole of the foot
- swelling to the heel
- tightness in the Achilles tendon.
What plantar fasciitis feels like
Plantar fasciitis usually causes a pain in the heel and along the bottom of your foot. The pain can vary from day to day and can be more painful depending on the type of activity you are doing and the time of day.
Some types of pain you experience may feel like:
- pain when standing from sitting or lying which can settle after walking for a few minutes
- dull, constant ache that varies throughout the day depending on activity levels
- sharp stabbing pain when using your foot or put any pressure through the heel
- pain following an increase in exercise, which may temporarily be relieved but comes back when you stop
- increased pain first thing in the morning after you have been lying down for a long period of time.
Causes
Any activity that irritates or damages your plantar fascia can cause plantar fasciitis, including:
- being on your feet for extended periods of time
- playing sports
- exercising or working on a hard surface floor
- exercising without stretching or warming up
- wearing shoes that don’t support your feet, such as flip flops or flat soled shoes
- walking or standing barefoot for long period of time
Medical conditions that can also cause plantar fasciitis include:
- high arched feet
- flat feet
- obesity (or a sudden increase in weight over a few months).
Diagnosing plantar fasciitis
We can diagnose plantar fasciitis with a physical examination and medical history of any ongoing foot problems. Typically pain and inflammation are present at the base of your heel.
Occasionally we may use diagnostic imaging if another issue or condition is causing the pain.
This diagnostic imaging may include:
- X ray
- ultrasound
- MRI scan.
Acute or chronic
Acute plantar fasciitis is the initial occurrence of symptoms which can present for up to 6 months. The symptoms will come and go during this time, but the condition often settles without our intervening too much. Gentle stretches and off the shelf insoles can be a beneficial form of treatment.
If symptoms persist for longer durations (longer than 6 months) and without relief, the initial acute condition can result in chronic condition. A chronic condition can be difficult to treat and may require a variety of treatments.
Treatment
We can manage this common condition with a variety of at home treatments as well as some over the counter medicine.
Once we have confirmed your diagnosis we may suggest one or more of the following treatments to help manage your condition and reduce your pain.
Stretching and massaging

There are numerous different ways to stretch. The most common are blocked calf stretches (see pictured), calf facia stretch and rolling stretch. This method of treatment is often used for long term treatment and can settle symptoms down in acute patients quickly.
Night splints
We may prescribe night socks (Strasberg socks) for you. These are long stockings that you wear at nighttime to allow a gentle but prolonged stretch of the plantar fascia while you sleep.
Orthotics (shoe inserts) or insoles
We may prescribe some gel insoles or arch supports that you can put in your footwear to help support your arch.
Supportive footwear
Supportive and well cushioned shoes will help support the arch of your foot.
Avoid wearing sandals, flip flops or flat shoes with no arch support.
Avoid walking barefoot.
Over-the-counter anti-inflammatory medicines
Non-steroidal anti-inflammatory medicines (NSAIDs), such as ibuprofen, can help reduce pain and inflammation. You can buy these without a prescription from many shops and supermarkets. Get advice from your GP or pharmacist if you use anti-inflammatories to reduce pain and inflammation.
Rest
If possible, for at least a week, limit or reduce the amount of sporting activity that you do and which can make your plantar fasciitis worse.
Ice
Ice the foot for at least 10 to 15 minutes twice a day to help reduce your inflammation. The cooling effect will also help with reducing pain in your foot.
Treatments for chronic plantar fasciitis
If your condition is chronic (it has been persistent for longer than 6 months), we can offer you other treatment options, providing that some of the above treatments have already been tried.
These options may include the following.
Extracorporeal shockwave therapy (ESWT)

This creates an inflammation response, which is said to increase the body’s own healing processes. Focused shockwaves are high energy acoustic waves that come together to achieve maximal energy at the target site. This overstimulates the nerves, which can reduce sensitivity and pain in chronic conditions.
ESWT is commonly used in patients who have not responded to more conservative treatments. A course of ESWT usually requires 1 treatment session a week for 3 follow on weeks. Ideally treatment will not take place any more than 2 weeks apart. This treatment method must incorporate a comprehensive rehabilitation programme.
Proximal Medial Gastrocnemius Release (PMGR)
This is a minimally invasive surgical procedure which involves releasing a small piece of fascia around the top of your calf to allow the muscle fibres to be released. Fascia is a thick band of tissue that runs from your heel to your toes on the bottom of the foot. We then close any subcutaneous (under the skin) layers and skin. We perform this technique to relieve tension in the Achilles tendon.
We usually perform this as a day case procedure the operating theatre. We generally use this procedure when all other non operative management options have failed. There are some typical complications which can occur after an operation, including:
- bleeding
- infection
- nerve damage
- DVT (deep vein thrombosis)
- wound healing problems
- return of the Achilles tendinopathy condition.
Steroid injection
In rare instances we may suggest a steroid injection into your plantar fascia. This injection can be painful and does not always work. We usually perform the injection using ultrasound guidance, to target the exact area for the injection.
This method of treatment has a short term effect, which means symptoms may resolve following the injection, but often return quickly. We can repeat these injections to improve symptoms, but the condition often persists.
Other steroid injection complications can include include:
- infection
- an increase in pain
- an increase in swelling
- ineffective treatment.
Contact information
Orthopaedic Outpatient Department