Neurodiversity information for parents and young people
About percutaneous drainage
If a patient has developed an abnormal collection of fluid inside their body, we insert a fine plastic tube, called a drainage catheter, into the fluid through a tiny incision (cut) in their skin. We use this tube to drain the abnormal fluid.
This procedure is called percutaneous (through the skin) drainage.
Why you need percutaneous drainage
A previous test has shown that you have developed an abnormal collection of fluid inside your body.
This abnormal buildup of fluid can lead to problems by pressing on nearby bodily structures or by harbouring infection.
Sometimes a fluid collection can disappear without treatment or with antibiotics alone. In your case, your doctors feel that we must remove the fluid promptly. This will improve your symptoms, speed your recovery and prevent further complications that might arise.
Your doctors and your interventional radiologist both feel percutaneous drainage is the best treatment option for you. They will discuss their recommendation with you and they will take your opinion into account. You will have the chance to ask questions. If, after discussion with your doctors, you do not want us to carry out the procedure, you can decide against it.
We will only go ahead with this procedure after you have given us your written consent.
Who performs the procedure and where it takes place
An interventional radiologist will perform the procedure. These doctors have special expertise in using X ray and scanning equipment and in interpreting the images produced. They use these images on screen to guide the procedure.
It will take place in the Kingston Hospital Radiology Department, either in the Interventional Screening Room or within the CT Scanner if this is more appropriate.
If a patient is too ill to be moved, we can perform it at the hospital bedside using portable equipment.
Preparing for your procedure
You may have the procedure as an outpatient or as an inpatient.
To prepare as an outpatient, do the following.
- You can take sips of water up to 2 hours before the procedure.
- You can take your normal medicines up until the procedure.
- When you receive your appointment letter, tell the Interventional Radiology Unit if you have previously had allergies to foods, medicines or intravenous contrast medium (the dye used for kidney X rays and CT scans).
- When you receive your appointment letter, tell the Interventional Radiology Unit if you have been on blood thinning tablets such as warfarin, aspirin or clopidogrel.
- We may give you some pre procedural painkillers and antibiotics if you need them.
If you are an inpatient, the following applies.
- You can take sips of water up to 2 hours before the procedure.
- You can take your normal medicines up until the procedure.
- We may give you some pre procedural painkillers and antibiotics if you need them.
If you are an outpatient
You must have a responsible adult go home with you.
You must also have a responsible adult to stay with you for 24 hours (including overnight).
When you arrive in the department, you will meet the team, including your nurse, interventional radiologist and radiographer. The radiographer operates the imaging equipment and is responsible for the images we take.
- We will ask you to put on a hospital gown and lie on the X ray or scanning table.
- We may place an intravenous cannula (a small flexible tube) in a vein on your arm to give you painkillers, sedation or antibiotics.
- We will wrap a cuff around your arm to monitor your blood pressure, and place a clip on your finger to measure your pulse and breathing.
- The doctor performing the procedure will choose the most appropriate point on your skin to approach the fluid collection. They will clean this area with antiseptic and anaesthetise it with an injection.
- We will guide a fine needle through this numb area, into the fluid collection, using the pictures from the scanner or X ray machine.
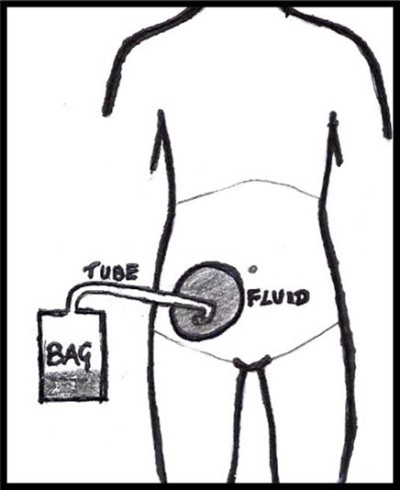
- Using a guidewire, we will exchange the needle for a plastic tube to drain the fluid to the outside. Sometimes all the fluid drains immediately and we can remove the tube. Usually we leave the tube in place to allow the fluid to continue to drain for the next day or two.
- If this is the case, we will connect the tube to a bag, secured with some stitches and covered with dressings.
Pain
After we give you painkillers and inject you with local anaesthetic, your skin and deeper tissues will go numb and the procedure should be almost painless.
If you do feel pain, the nurse looking after you will be able to arrange stronger pain relief and sedation.
How long it takes
The whole procedure takes about 40 minutes. Most of this time is spent in preparation; inserting the tube itself takes about 10 minutes.
After the procedure
After the procedure we will transfer you back to your ward or the Radiology Day Ward.
It is important that you remain comfortable and lie quietly in bed for a few hours until you have recovered.
Your nurses will keep a close eye on you by monitoring your pulse, blood pressure, breathing and temperature, to ensure you are recovering as expected.
Your drainage tube is important for your recovery
Your nurse will check the bag regularly, to monitor how much fluid is draining and to prevent the bag becoming too heavy.
- Avoid pulling the tube out by accident while it remains in place.
- Avoid sudden movements.
- Always make sure that the attached bag can move freely with you.
- Avoid getting the tube twisted or pulled.
- Let your nurse know immediately if you think the tube has been pulled in any way.
How long the tube stays in
The length of time the tube stays in varies and will depend on the underlying cause for your fluid buildup. The tube may only need to stay in for a short time, but you may need further scans to check the fluid has been drained satisfactorily.
When we remove the drainage catheter, it is usually a simple procedure done on the ward, and it rarely causes too much discomfort.
Risks
Percutaneous fluid drainage is a safe procedure, and there are few serious risks, but the following may occur.
- Damage to nearby bodily structures as we guide the tube into place.
- Bleeding. It is rare for this to cause a serious problem.
- If the fluid collection is infected, some infection can spread into your blood stream and give you a shivering attack. We generally treat this satisfactorily with antibiotics.
- Sometimes the fluid is too thick, or has gathered into small pockets, making it hard for it to drain out of a single tube. If this happens we may insert further tubes, or perform an operation if the fluid is particularly stubborn.
If you have concerns or questions about this procedure, you can discuss these with your medical team and your interventional radiologist at any time.
Contact information
Interventional Radiology Unit
Interventional Radiology Unit Charge Nurse
Telephone:
Interventional Radiology Unit: 020 8934 6206
Interventional Radiology Unit Charge Nurse: 020 8934 2758