Neurodiversity information for parents and young people
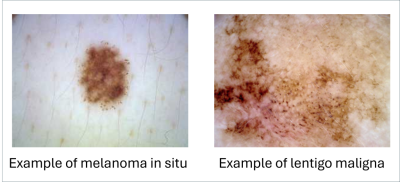
About melanoma in situ (MIS)
MIS is the earliest stage of a skin cancer called melanoma. ‘In situ’ means that the cancer cells have not had the opportunity to spread to anywhere else in your body.
If you are diagnosed with MIS it means there are cancer cells in the top layer of your skin (the epidermis) but they have not started to spread or grow into deeper layers of the skin. This is why some doctors call in situ cancers ‘pre cancer’.
Lentigo maligna (LM)
Lentigo maligna (LM) is a type of melanoma in situ (MIS).
LM is a slow growing lesion (area of skin damage) that appears in areas of skin that get a lot of sun exposure, such as the face or upper body. LM can take years to develop.
Similar to MIS, lentigo maligna cells have not had the opportunity to spread to anywhere else in your body. If you are diagnosed with LM it means there are cancer cells in the top layer of your skin (the epidermis) but they have not started to spread or grow into deeper layers of the skin.
The health outlook for anyone with MIS is excellent.
Causes
The sun’s ultraviolet (UV) radiation is a key factor in the development of MIS. Sunbeds are also an important factor.
Studies suggest that children under the age of 15 years who have episodes of sunburn (redness of the skin) increase their risk of developing MIS when they are older.
Studies also suggest that episodes of sunburn as an adult, for example on holiday or during leisure time, may play a key role in causing MIS.
Continuous exposure to the sun is also a risk.
It is important to take preventative measures to lower your risk of developing invasive cancer(s). See ‘How to protect your skin’ below.
How MIS and LM are treated
MIS is treated with surgery. If it is not treated with appropriate surgery, it can develop into an invasive cancer and possibly spread to other parts of your body.
We aim to surgically remove the cancerous cells fully for diagnosis and treatment. When we remove these cells, we also take a narrow border of healthy tissue from around your MIS.
We cover your wound with a dressing and give you post operative care instructions.
If the area we remove is large, we may need to use a skin graft or another type of plastic surgery to close it.
You may be uncomfortable for some days after your operation. Paracetamol is a common over the counter painkiller which works well to reduce pain after surgery. Take 2 paracetamol tablets every 6 hours. Your doctor or nurse will offer relevant advice on pain relief during your appointment.
Do not take aspirin or anti inflammatory drugs such as ibuprofen because they increase the risk of bleeding.
Do not drink alcohol because this will increase the risk of bleeding.
LM is treated with surgery, immune response cream or radiotherapy. If it is not treated, it can develop into a more serious disease.
We will discuss treatment options with you so you can make the right choice.
Outlook after treatment
The outlook for patients is excellent after treatment for MIS.
Most patients only need to return to clinic once before we discharge them.
How to protect your skin
To protect yourself you must examine your skin every month to look for any noticeable changes. This will help to detect early warning signs of MIS.
Check for existing or new skin lumps or moles that get bigger, change colour, bleed or itch. Most changes are harmless but they may indicate the start of a skin cancer.
![]()
Protecting your skin from the sun can reduce your risk of getting MIS.
Follow these recommendations.
- Protect yourself from the sun between 11am to 3pm (when the sun is at its strongest).
- Wear protective clothing: hat, long sleeves, long skirt or trousers.
- Apply a sunscreen regularly to exposed skin before going into the sun. Use a brand with sun protection factor of 30 or above which can also block both UVA and UVB light. Re-apply the sun cream according to the manufacturer’s recommendations, especially if you are sweating or have been swimming when you are out in the sun.
- Protect your children from the sun in the same way.
- Avoid artificial sunlamps, including sunbeds and UV tanning cabinets.
- Be skin aware. Examine your own skin every few months.
Photographs courtesy of dermnetnz.org
More information
Kingston Hospital Skin Cancer Clinical Nurse Specialist (CNS).
Tel: 020 8934 3002 or email on khft.
NHS on skin cancer (including videos)
British Association of Dermatologists on MIS
NHS video on skin cancer self examination
Macmillan: general advice on cancer support services offered nationwide
Macmillan: advice on benefits and financial support
Cancer Research UK on skin cancer
SKCIN (Karen Clifford Skin Cancer Charity) on skin cancer
Melanoma Focus on skin cancer
Cancer Care Map: find cancer support services near you
Cancer Wellbeing London: health and wellbeing events in your area
Contact information
Kingston Hospital dermatology & plastic surgery admin
Kingston Hospital skin cancer nursing team and Macmillan support worker, Monday to Friday 9am to 5 pm. Email: khft.
Kingston Hospital Cancer Counselling Service, Monday to Friday 9am to 5pm. Email: khft.
Kingston Hospital Macmillan Cancer Information and Support Service, Monday to Friday 9 am to 5 pm. Email: khft.
Royal Marsden Hospital, Sutton Clinical Oncology and Radiology, Monday to Friday 9am to 5pm
Telephone:
Kingston Hospital dermatology & plastic surgery admin: 020 8934 6473
Kingston Hospital skin cancer nursing team and Macmillan support worker: 020 8934 3002
Kingston Hospital Cancer Counselling Service: 020 8934 2114
Kingston Hospital Macmillan Cancer Information and Support Service: 020 8973 5001
Royal Marsden Hospital, Sutton Clinical Oncology and Radiology: 020 8661 3374