Demo page for boxes, columns and icons
About Kingston Healthy Weight Centre
|
Please note there is currently a national shortage of weight loss injections. If your referral to KHWC is accepted, we will invite you for an initial assessment appointment and, if the multidisciplinary team feel that weight loss injections would be appropriate for you, we will place you on a waiting list. We are currently not able to prescribe weight loss injections. If the situation changes, we will update this information (14 September 2024). |
KHWC provides a comprehensive surgical and medical service. Its primary aim is to improve the health of patients who are overweight and have medical problems that can be helped with weight loss.
These conditions include diabetes, obstructive sleep apnoea and high blood pressure.
| We offer two treatment pathways: |
|---|
|
Pathway 1: weight loss surgery (also known as ‘bariatric’ or ‘metabolic’ surgery) Pathway 2: weight loss medicines |
Weight loss surgery and weight loss medicines are highly specialised interventions.
We only recommend them for use with people who are significantly overweight and have been unable to lose weight or maintain weight loss with other weight loss interventions.
To been seen by the KHWC, you must be referred by your GP or other hospital doctor.
Other weight loss options
If you feel these two options are not for you, there are other services available to support you with weight loss.
You may be able to access these options yourself or through your GP. They include:
- The NHS Better Health 12 week weight loss programme which you can download for free (see More information section below).
- Local commercial weight loss groups such as WeightWatchers or Slimming World (see More information section below).
- Some local boroughs provide access to weight loss programmes. These may include slimming groups, digital weight management programmes and Exercise on Referral schemes for free or at a reduced cost. Contact your GP to find out about the options available in your local area.
- Your GP may be able to refer you to a dietitian at their GP practice, or at your local hospital.
- Your GP may be able to prescribe a weight loss medicine called orlistat (also known as Xenical).
The KHWC team
The KHWC multidisciplinary team (MDT) includes the following:
- a specialist nurse
- consultant bariatric (obesity) surgeons
- consultant bariatric anaesthetists
- consultant endocrinologists (hormone specialists)
- a specialist dietitian
- a psychologist (mental health professional).
What happens when you are referred to KHWC
You can expect the following after you are referred.
- After we have received and accepted your referral, we will ask you to attend an appointment at our metabolic assessment clinic. At this appointment you will meet the specialist nurse or other members of the KHWC MDT. They will discuss different treatment options with you. They will also give you a blood test. Allow at least 1 hour for this appointment.
- Following your appointment at the assessment clinic, our team of specialists will meet to discuss the best treatment options for you.
- If we think you are suitable for the treatments we offer, they will ask you to attend further appointments with other MDT members. You will see the surgeons or endocrinologists, depending on which pathway you choose. We will offer you dietary support from the dietitian in group sessions. We may ask you to meet with our psychologist and come in for further investigations. These can include sleep studies, an endoscopy (a test to look at your digestive tract) or an echocardiogram (a scan to look at your heart).
- When you have met the appropriate members of our MDT, we will make a final decision about your treatment.
- You may not be an appropriate candidate for all treatments. We will make sure that you have all the information you need to make an informed choice. We will discuss this with you fully at your appointment. Together we can discuss which pathway would be best for you.
- If appropriate, it may be possible for you to change to a different pathway if you change your mind or if your circumstances change.
|
Our service follows national clinical guidelines for weight loss surgery and medicines set out by the National Institute for Health & Care Excellence (NICE) and British Obesity & Metabolic Surgery Society (BOMSS). These specify eligibility requirements for the different treatments available. |
Important to remember
It is important to remember that whatever weight loss treatment you have, it is only a tool to aid weight loss. Your long-term success depends on your commitment to change the way that you eat and what you eat, and follow a healthy lifestyle. This starts at your first assessment appointment.
Pathway 1: weight loss surgery
Weight loss surgical treatment (‘bariatric’ or ‘metabolic’ surgery)
Weight loss surgery is used to help people who are significantly overweight. It is a lengthy process and we offer it to people who have not been able to achieve or maintain weight loss through diet and exercise alone.
- Weight loss surgery makes your stomach smaller and changes the hormones that your body produces when you eat. This reduces the amount you can eat and makes you feel fuller sooner.
- Some types of surgery also reduce the nutrients and calories that your body absorbs from the food you eat.
- The main aim of surgery is to help reduce the health problems that are associated with being significantly overweight, rather than reaching an ‘ideal’ weight.
- When coupled with healthy eating and lifestyle changes, surgery can ultimately improve your health. It can also reduce or eliminate your use of some medicines and improve your quality of life.
- Wherever possible, weight loss surgery is carried out using laparoscopic (keyhole) procedures while you are under general anaesthetic.
- Patients usually go home 1 to 3 days after surgery.
- It usually takes 4 to 6 weeks to recover and resume everyday activities.
Commitment and motivation
![]()
- We do not set a target for weight loss prior to your surgery. We do ask that you start to make changes to your diet and lifestyle before surgery. This will give you the best chance of success, and we will support you in doing it.
- If you gain weight between your assessment appointment and your surgery date we will examine the reasons for this. We will reassess whether surgery is the most suitable route for you.
We require you to attend all of your appointments. This will avoid delays in your assessment process, enable us to monitor any serious complications after surgery and help you meet your personal goals.
The amount of weight loss varies from person to person. It depends on the surgical procedure used and on how well you manage to make diet and lifestyle changes to support your surgery.
On average people lose 20% to 30% of their total body weight after the type of surgeries we offer at KHWC.
- Most people usually lose weight rapidly in the first 6 to 9 months after surgery.
- Their rate of weight loss then slows and levels off between 12 to 18 months after surgery.
Important information
Weight loss surgery does not take away your desire to eat.
To support your surgery, it is essential to change the way you eat, make healthy food choices and increase your activity levels.
Failure to do this can result in disappointing weight loss and weight regain.
Benefits
Weight loss surgery can be a useful tool, along with dietary and lifestyle changes, for someone who struggles to lose weight or maintain a healthy weight.
Weight loss can often help to reduce weight related complications such as type 2 diabetes, high blood pressure, sleep apnoea and osteoarthritis. It can also reduce reliance on the medicines used to treat these conditions.
Risks
All weight loss surgery is associated with certain side effects and risks. See the Possible Complications sections below.
All types of surgery come with a risk of mortality (death). The risk varies depending on factors such as any illnesses you suffer from, your age, the complexity of your surgery and surgeries you may have had previously.
At Kingston Hospital we offer two types of weight loss surgery:
- Gastric sleeve (sleeve gastrectomy)
- Gastric bypass (two types)
Deciding which surgical option is best for you
We make all of our surgical choices based on the patient’s medical conditions and suitability.
We discuss each patient at our regular MDT meetings. This ensures the whole KHWC team has a complete understanding of each patient’s situation before we make any treatment decisions.
Use the next drop down menus to learn more about gastric sleeve and gastric bypass.
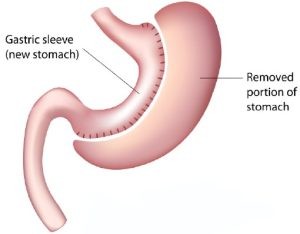
A sleeve gastrectomy operation reduces the size of the stomach. We achieve this by stapling the stomach along its length and removing the excess portion, leaving a long tube or sleeve.
The stomach that remains is considerably smaller and this significantly reduces the amount of food that you can eat.
It can also affect the hormones which regulate your appetite, thus making you feel less hungry.
| Outcome of gastric sleeve |
|---|
| On average people lose 20% to 30% of their total body weight after 2 years. |
Possible complications of sleeve gastrectomy
Possible complications include:
- leaking from the staple line (along the join made during surgery)
- bleeding from the staple line (along the join made during surgery)
- kinking or narrowing of the stomach causing vomiting or difficulty swallowing
- development of gallstones due to rapid weight loss. On rare occasions, a patient may need a further operation to remove their gallbladder.
- vomiting is common if you eat too quickly, eat too much, or take food and fluid together
- nutritional deficiencies (shortages) such as lack of vitamin B12, iron and calcium. You will need to take nutritional supplements for the rest of your life.
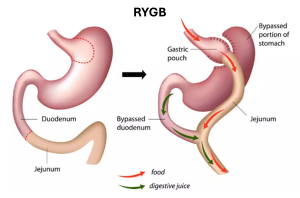
1. Roux en Y bypass (RYGB)
- In this surgery the surgeon staples across the stomach to create a small pouch. The ‘new’ stomach is similar in size to an egg cup.
- The small intestine (which carries food away from the stomach) is cut and then brought up and attached to the small pouch.
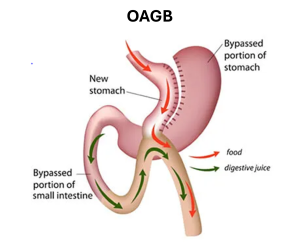
2. One anastomosis gastric bypass or OAGB (mini bypass)
- This involves stapling the stomach to create a small, elongated new stomach (pouch). This pouch is detached from the main part of the stomach.
- A loop of small bowel is then lifted up and connected to the pouch.
- The rest of the stomach remains but food does not enter it. The digestive juices from the pancreas mix with the food coming from the small pouch.
| Outcome of gastric bypass (both types) |
|---|
| On average, people lose 20% to 30% of their total body weight body weight over 2 years. |
Both the Roux en Y gastric bypass and OAGB work through a combination of mechanisms, as follows.
- The newly created stomach pouch is considerably smaller, which restricts the volume of food that you can eat.
- Signals that come from the gut are altered. This leads to increased levels of fulness and reduced hunger.
- Some of the small bowel is bypassed. This reduces the amount of calories, protein and other nutrients that you can absorb.
Possible complications of gastric bypass (both types)
Possible complications include:
- strictures: a narrowing at the surgical joins at the top and bottom of the stomach. This may require another procedure: endoscopic (using a tiny camera) or surgical. This widens the area and allows food to travel through at the correct rate.
- leakage or bleeding from the join between the stomach and intestine
- ulcers (open sore on the lining of your stomach)
- perforation (tear)
- internal hernia (small bowel or intestine intrudes into your abdominal cavity)
- nutritional deficiencies such as vitamin B12, iron and calcium. You will need to take nutritional supplements for the rest of your life.
- gallstones due to rapid weight loss. On rare occasions, if you develop these we may need to give you a further operation to remove your gallbladder.
- ‘Dumping syndrome’. Some people develop this condition if they eat too much fat or sugary food or drink, or if they eat and drink at the same time. It can cause unpleasant symptoms including nausea, vomiting, diarrhoea, sweating, faintness, weakness and an increased heart rate.
- Vomiting can occur if your portions are too large, if you do not chew your food properly, or if you take food and fluid together.
All types of weight loss surgery require you to follow some dietary guidelines. These are to:
- Follow a special diet before your operation and for the first few weeks after surgery.
- Follow recommended eating techniques for the rest of your life.
- Take vitamin and mineral supplementation for the rest of your life.
- Attend regular follow up appointments for the rest of your life.
All types of weight loss surgery affect what you will be able to eat and how much you can eat.
The KHWC team will discuss this with you if you decide you would like to be considered for weight loss surgery.
If you have weight loss surgery we will ask you to follow a special diet before your operation and a different special diet after your operation.
Use the next drop-down menus to learn about the pre-operative diet and the post-operative diet.
- In the 2 to 4 weeks prior to your surgery you will need to follow a ‘liver shrinkage diet’. This is so that the surgeons can (temporarily) move your liver so they can safely access your stomach.
- We will ask you to maintain a low calorie diet (about 1000 calories per day). This can be based on normal foods, or milk only or Slimfast only.
- If you do not strictly adhere to the diet, the surgeon may decide it is too risky to go ahead with your surgery. We will discuss this with you in detail if you decide to undergo surgery.
In the 6 weeks after your surgery you will need to follow a process of gradual reintroduction of food.
This will allow the new pouch to heal, avoid the new stomach overstretching and reduce side effects such as nausea and vomiting.
| Weeks | Food and drink allowed |
|---|---|
| 1 to 2 | Fluids only, for example water, milk, soup with no bits |
| 3 to 4 | Smooth pureed food |
| 5 to 6 | Soft foods, for example flaked fish, soft vegetables |
| 7 onwards | Gradual return to normal food texture and small portions of a healthy, balanced diet |
If you have weight loss surgery it will be essential that you make some changes to your eating technique. These are important to help to reduce side effects such as discomfort, nausea and vomiting.
You will only be able to manage small portions of food. It is a good idea to serve up smaller portions using a side or child’s plate.
You will need to eat slowly and chew your food well. We recommend you chew 20 to 30 times per mouthful.
You cannot eat and drink at the same time because this will cause you to be sick. You will need to drink fluids at separate times from mealtimes.
There are some foods that people commonly struggle to eat after weight loss surgery. They can get stuck when you eat them and make you feel uncomfortable. They include:
-
fibrous, dry meats
- bread
- rice
- stringy, fibrous vegetables.
Fizzy drinks
- Avoid fizzy drinks after surgery because they can cause bloating and discomfort.
Alcohol
- We recommend you avoid alcohol for the first few months after your surgery to avoid irritation to your healing stomach.
- Weight loss surgery can affect how you respond to alcohol and can lead to unwanted effects and alcohol dependency.
- Alcohol can delay wound healing immediately after surgery and can lead to weight regain in the long term.
- If you want to include alcohol after a few months we advise you to only drink small amounts.
Vitamin and mineral supplements
Weight loss surgery can lead to malnutrition if you do not follow a balanced diet.
You will need to take vitamin and mineral supplements every day for the rest of your life after surgery. This is to prevent nutritional deficiencies which can lead to conditions including:
- anaemia (low iron leading to low red blood cells)
- osteoporosis (weak bones and bone fractures)
- muscle weakness
- nerve damage (which can lead to problems such as muscle weakness, confusion and memory loss).
You will need to take the following:
- multivitamins and minerals once or twice a day
- additional calcium, vitamin D and iron
- vitamin B12 injections every 3 months.
Some of these are unavailable on prescription so you will have to buy them yourself from pharmacies or supermarkets.
Regular follow up appointments
You will need regular blood tests in the first 12 months after surgery, then at least annually for the rest of your life.
You will also need to attend appointments with the nurse, surgeon and dietitian to monitor you for potential complications and for nutritional deficiencies.
Weight loss surgery requires you to commit to making dietary and lifestyle changes to make sure you achieve the best outcome from your surgery.
The process leading up to surgery can take several months. This is because it is vital that you are in the best possible condition (medically and psychologically) before surgery. This will ensure you are safe and you achieve the best possible results.
After surgery you will be under the care of the KHWC for 2 years. We will then hand over your care to your GP.
Before surgery
- We will ask you to attend further assessment appointments with the surgeon and anaesthetist. They will discuss the procedure with you in more detail and assess your suitability for surgery and anaesthetic.
- We will also ask you to attend education sessions and appointments with the dietitian. This is so you can discuss your current diet and the dietary changes that you will need to make before and after surgery.
- Some people may need to see other specialists before surgery (for example a psychologist – mental health professional – or sleep specialist). They will assess whether there may be medical or psychological issues that could impact on the outcome of your surgery.
- We will wait for the outcome of these appointments before making a final decision about surgery.
After surgery
- After surgery, you will have follow up appointments with us to make sure you are managing your eating and drinking well, and healing well.
- During the 2 years following your surgery we will make appointments for you to see the specialist nurse, the surgeon and the dietitian. They will monitor your nutritional status and assess you for any problems.
- After this time your GP will be in charge of monitoring your care. They can refer you back to the KHWC if you develop any problems.
Other factors to consider when making your decision
Use the drop-down menu for information on other factors to consider when making your decision.
Pregnancy after weight loss surgery
- Losing weight can increase your fertility. We advise you to avoid pregnancy for 18 to 24 months after surgery, until your weight has stabilised.
- Rapid weight loss after weight loss surgery can put your baby’s development at risk.
- Certain types of contraception may be less effective after weight loss surgery.
![]()
Speak to your GP or family planning clinic about the most suitable form of contraception for you.
Smoking
- Smoking increases your risk of complications during and after surgery.
- All patients undergoing surgery need to stop smoking for at least 6 months before we put them on the waiting list.
|
The purpose of weight loss surgery is to help improve your health, life expectancy and quality of life. Smoking is the single most detrimental activity that you can undertake to affect your health. It is the biggest cause of death and illness in the UK. |
Hair loss
- Hair loss is quite common in the first year after weight loss surgery. This is generally temporary and only lasts while you are losing weight rapidly.
Excess skin
- Significant weight loss can result in loose skin in some areas of your body (for example around your tummy, arms, legs and breasts).
- Some people are not bothered by this and others find it upsetting. Occasionally, if skin folds are difficult to keep clean and dry, they become infected or sore. Plastic surgery is only way to effectively deal with loose skin, but it is not usually funded by the NHS.
Pathway 2: weight loss medicines
If you feel a medical pathway for weight loss is more appropriate for you, our consultant endocrinologist will see you to assess your suitability for weight loss medicines.
KHWC offers weight loss medicines which are approved by NICE for prescription in NHS specialist weight management clinics. The medicines currently approved for prescription are detailed below.
Note these are subject to change as and when NICE guidelines are updated (and subject to availability from manufacturers).
NICE guidelines make specific recommendations about how these medicines can be prescribed, based on:
- Suitability for the patient, based on specific BMI thresholds and the presence of weight related health conditions. Your endocrinologist will follow these guidelines and advise which medicines would be appropriate for you.
- Use of these medicines only if accompanied by a reduced calorie diet and increased physical activity.
The main category of medicines currently approved for specialist weight management clinics to prescribe are called ‘GLP 1 receptor agonists’ (GLP 1RAs). These act like the hormone GLP 1 which we produce naturally in our bodies and which affects appetite and food intake.
These medicines do the following:
- Help the body produce insulin (a hormone that enables your body to use glucose for energy).
- Reduce the amount of excess glucose (sugar) being released by your liver.
- Slow the rate at which your stomach digests and empties food making you feel fuller.
- Reduce your appetite, resulting in reduced food intake.
Some of the medicines also act like other hormones in our bodies that affect your appetite and help to keep your blood sugar stable.
GLP 1RAs come in pre-filled pens that you use to inject yourself into your abdomen, thigh or upper arm once a week.
We will initially prescribe you with a low dose. We increase this gradually to a recommended maintenance dose over several weeks, to minimise side effects.
Commitment and motivation
![]()
It is important to remember that weight loss medicines are only a tool to aid weight loss.
Your long-term success depends on your commitment to change the way that you eat and what you eat, and follow a healthy lifestyle.
This starts at your first assessment appointment.
In research studies, people taking the maintenance dose of GLP 1RAs and following a reduced calorie diet combined with increased activity, lost an average of around 15% to 20% of their body weight, depending on which medicine they were using. They lost this weight over about 16 months.
| Action | Period of time | Average weight loss |
|---|---|---|
All of these combined:
|
16 months | 15% to 20% of body weight |
Note this is an average, so some people lost more than this and some people lost less.
![]()
Current NICE guidelines say that GLP 1RA injections can be prescribed for weight loss for 2 years. Research shows that people are likely to regain weight when injections are stopped.
Benefits
Studies show that people who combine GLP 1RAs with a healthy diet and exercise also experience the following:
- reduction in the risk of heart disease
- improvements in blood pressure and kidney function
- improved physical function
- better quality of life.
Side effects and risks
As with any medicines, there are some potential side effects. For most people, these side effects settle down a few weeks after starting weight loss injections. Some people are not able to tolerate the medicines so they have to stop taking them.
The most common side effects of GLP 1RA medicines include:
- nausea
- vomiting
- burping
- constipation
- diarrhoea
- dizziness
- tiredness
- gastrointestinal (stomach) discomfort
- reflux (stomach acid travels out of the stomach back into the oesophagus or food pipe)
- hypoglycaemia (low blood sugar) when used in combination with some diabetes medicines such as insulin or sulfonylureas.
Other serious but less common side effects include:
- gallstones
- pancreatitis (inflamed pancreas)
- altered taste
- changes in vision.
Stop taking the medicine if you begin to note symptoms of acute pancreatitis such as severe abdominal pain, yellowing of the eyes or skin, or pale grey or white coloured stools (poo).
Some medicines in this category can also increase the risk of medullary thyroid cancer.
For most people the side effects are mild and reduce over time.
![]()
Contact the KHWC team or come to Kingston Hospital Emergency Department (A&E) if symptoms persist or become severe.
Symptoms include:
- severe abdominal pain that will not go away
- vomiting or diarrhoea that does not stop
- yellowing of the skin or eyes
- pale grey or white coloured stools
- a lump or swelling in the neck
- hoarseness
- trouble swallowing
- shortness of breath.
To help yourself lose weight you will need to do the following.
Follow a reduced calorie diet and do more exercise
Studies show that people get the most benefit from weight loss medicines when they follow a reduced calorie diet and increase the amount of exercise they do.
We will invite you to attend group sessions with the specialist dietitian. They will offer advice and support on making dietary changes to help you lose weight with the injections, maintain this weight loss and prevent weight regain.
In accordance with NICE guidelines, KHWC will consider discontinuing weight loss injections if you do not achieve a 5% weight loss 6 months after starting the medicine.
After your assessment appointment we will offer you a series of further appointments with other members of the MDT.
Your endocrinologist will do the following.
- Discuss the treatments available with you in more detail and assess your suitability.
- Provide prescriptions for the appropriate weight loss medicines. These will be provided based on information that you will be asked to confirm each month, such as your weight, any side effects and your eating patterns.
- Monitor your progress and assess for any side effects or complications.
Your specialist dietitian will provide the following.
- Dietary assessment and tailored advice to support you to start making dietary changes before we prescribe medicines. This will be in a group session (or face to face in exceptional circumstances, for example you suffer from binge eating disorder, you have a diagnosis of a learning disability or you need an interpreter).
- Diet and lifestyle advice to support your weight loss during treatment and help minimise weight regain when treatment finishes. We may offer this via online group sessions or on an individual basis if required.
Some people may need to see other specialists (for example a psychologist) before starting medicines. This is to assess whether there may be medical or other issues that could impact the suitability of weight loss medicines.
In these situations we will await the outcome of these appointments before making a final decision about prescribing medicines.
Your GP will take charge of monitoring your care after 2 years of treatment, when your prescription comes to an end (or sooner if your medicine is stopped earlier).
Other factors to consider when making your decision
Use the drop-down menu for information on other factors to consider when making your decision.
Stop smoking
We strongly advise you to stop smoking before starting weight loss medicines.
We understand that stopping can be difficult and you may need support. There are many support organisations available that we can discuss with you.
|
The purpose of prescribing weight loss medicine is to help improve your health, life expectancy and quality of life. Smoking is the single most detrimental activity that you can undertake to affect your health. It is the biggest cause of death and illness in the UK. |
Contraception and pregnancy with weight loss medicines
Losing weight can increase your fertility.
Do not use GLP 1RA medicines during pregnancy because their effects on an unborn baby are unknown.
- Stop your GLP 1RA medicines at least 2 months before a planned pregnancy.
- GLP 1RA medicines can affect the absorption of oral contraceptives.
- Use other suitable methods of contraception while you are using weight loss injections.
![]()
What happens now
If you feel bariatric surgery or weight loss injections are right for you, wait to hear from the KHWC with your medical assessment clinic appointment.
We are experiencing a high volume of referrals so it may take a few weeks before you receive your appointment.
If you do not wish to proceed with weight loss surgery or injections, contact the KHWC to let us know (see Contacts section below).
For further support, see the ‘Other weight loss options’ section at the top.
More information
Books on weight loss (bariatric) surgery
- Recipes for Life before and after a sleeve gastrectomy or gastric bypass by Nutrition and Diet Resources UK. To buy online
- Living With Bariatric Surgery (2018) by Denise Ratcliffe
- Cut Down to Size: Achieving success with weight loss surgery (2013), by Jenny Radcliffe
- Return to Slender After Weight loss Surgery: Mouth-Watering Dishes to Nourish, Feed and Inspire You (2010), by Carol Bowen Ball (Kindle only)
Other resources
Weight loss
NHS Better Health Weight Loss Programme (free download)
NHS on how to calculate your BMI
Weight loss surgery
British Obesity and Metabolic Surgery Society on weight loss surgery
IFSO on:
Food and eating
British Dietetic Association on:
British Heart Foundation on:
NHS food facts and recipe ideas
BDA information on mindful eating
Smoking
Exercise
Versus Arthritis on exercises for people with arthritis
Information on Better Bones: an exercise programme people with arthritis or osteoporosis with a GP in Kingston borough or who live or work in Kingston borough
Contact information
Kingston Healthy Weight Centre
Email: khft.khwcbariatrics@nhs.net