Children's Community Nursing Service, Richmond
Making a decision
This document is called a decision-aid. It will help you decide between different options for the birth of your baby.
It is for women who have been recommended an induction of labour because labour has not started by 41 to 42 weeks.
We recommend you go through this information and then talk to your midwife or obstetrician to discuss your options. You might also want to write down and talk about your preferences and concerns so we know what matters to you.
At Kingston we are committed to supporting your choices for your birth.
Your options
Most people go into labour naturally between 37 and 42 weeks.
We recommend planning an induction if you reach 41 weeks of pregnancy and labour has not started naturally.
An induced labour is one that is started artificially. People often call it 'being induced'. About 1 in 3 labours in England are started in this way.
There are several reasons why you may be offered an induction. This decision-aid is concerned with induction that is offered because your pregnancy has continued beyond 41 weeks. If you are being offered an induction for another medical reason, you will have a discussion with your obstetrician.
It is your choice whether to have your labour induced. You might find it helpful to use the BRAIN tool to help you decide. If you decide not to be induced, you can talk to a doctor or senior midwife to make another plan.
For more information about how a labour is induced, read our information on The induction journey: your options. You can also attend our online Induction of Labour workshop (see below).
Decision-making using the BRAIN tool
BRAIN is a way of helping you gather the information you need to make informed decisions about your and your baby’s health.
BRAIN stands for:
B – Benefits
What is the benefit of having this procedure or intervention?
R – Risks (or disadvantages)
What are the risks of this process or intervention for me and my baby?
A – Alternatives
What is the alternative to this procedure or intervention? Is there another option?
I – Instinct
What do you feel is right for you?
N – Nothing
What happens if I do nothing? Is there more time for me to decide?
Benefits
Why we recommend induction
There are two main reasons why induction is recommended when pregnancy lasts longer than 41 weeks:
- to reduce the very small chance of the baby dying before it is born (called a stillbirth)
- to reduce the very small chance that the baby needs care in the intensive care unit because they are not well at birth.
Still birth
Most babies born in the UK are healthy at birth.
However, as pregnancy continues, the chance of stillbirth increases gradually. At around 42 weeks, it increases more significantly.
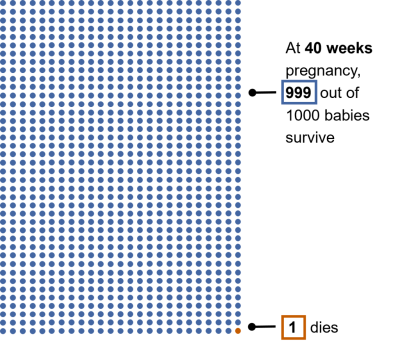
At 40 weeks of pregnancy, out of 1000 births, approximately 1 baby will be stillborn and 999 will survive.
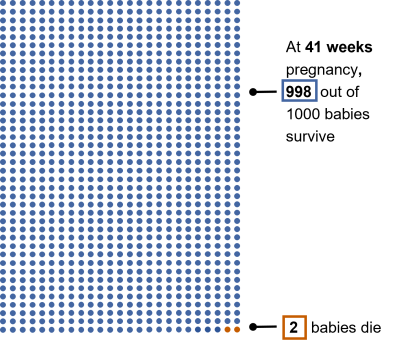
At 41 weeks of pregnancy, out of 1000 births, approximately 2 babies will be stillborn and 998 will survive.
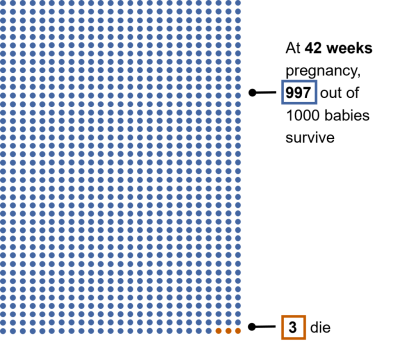
At 42 weeks of pregnancy, out of 1000 births, approximately 3 babies will be stillborn and 997 will survive.
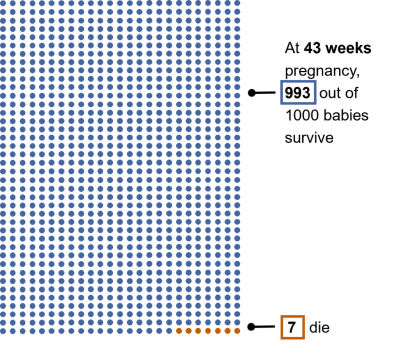
At 43 weeks of pregnancy, out of 1000 births, approximately 7 babies will be stillborn and 993 will survive.
Unfortunately, it is not possible to predict which babies will be affected. We recommend induction by 42 weeks to reduce the overall number of stillbirths.
We cannot calculate your baby’s individual risk of a stillbirth. Important factors that will affect the risk include your age, weight, general health and whether you have had a baby before.
Intensive care
The chance of your baby needing to go to intensive care is very small. However, that chance increases the longer we wait to induce labour after 41 weeks.
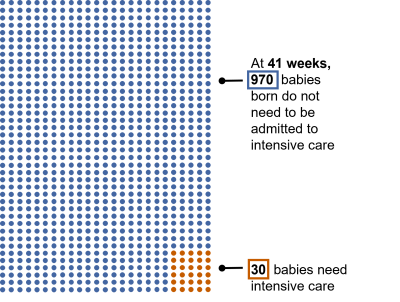
At 41 weeks of pregnancy, out of 1000 births, around 30 would be admitted to intensive care and 970 would not need to be.
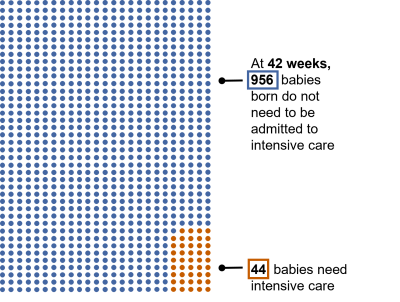
At 42 weeks of pregnancy, out of 1000 births, around 44 would be admitted to intensive care and 956 would not need to be.
Other benefits
Compared to waiting beyond 42 weeks, an induction before 42 weeks:
- may reduce the chance of needing an unplanned Caesarean
- may increase the chance of having a vaginal birth
- may lower the chance of having a heavy bleed immediately after the birth
- may lower the chance of having a severe perineal tear (a tear that affects the back passage or anal sphincter), although the overall chance of this kind of tear is low.
Risks (or disadvantages)
Being induced may affect your labour and birth experience.
How you give birth
Your chance of having a straightforward vaginal birth is highest:
- if you go into labour spontaneously before 42 weeks
- and you plan to give birth in the Birth Centre or at home.
An induction may increase the chance of an assisted vaginal birth with either forceps or a ventouse suction cup. This is particularly the case if you have an epidural (a pain-numbing injection in your back. You can read more about epidurals ). It is also more likely if you are having your first baby.
Choices about where you give birth
An induction means you are more likely to give birth in the Delivery Suite. This is because you may be recommended things that are not available in the Birth Centre or at home.
The Delivery Suite provides all women in labour with their own room, bathroom and midwife. Their overall care is managed by doctors. The baby's heartbeat can be monitored continuously. If needed, a "hormone drip" may be recommended as part of the induction process. This drip is intravenous oxytocin, which increases the frequency and strength of contractions.
The Birth Centre provides all women in labour with their own room, bathroom and midwife. Their overall care is managed by midwives. The baby's heartbeat is monitored at regular intervals, using a "sonicaid" or hand-held doppler. The rooms are designed to have a "home-from-home" environment, with minimal medical equipment. The "hormone drip" is not available.
You can read more about where you can give birth.
You may be able to have an induction in the Birth Centre if you do not need the hormone drip and your pregnancy is uncomplicated.
Pain relief choices
Women are more likely to ask for an epidural if labour is induced with a hormone drip. This is because contractions can feel more intense. An epidural is available in the Delivery Suite but not in the Birth Centre.
Birthing pools are available in the Birth Centre (in three rooms) and the Delivery Suite (in one room). If labour progresses without the need for the hormone drip, the pool may be an option. If the hormone drip is suggested, using the birthing pool is not recommended.
All other types of pain relief, including Gas and Air (Entonox) and pethidine, are available whether labour is induced or spontaneous.
Vaginal examinations
An induction is likely to involve more vaginal examinations than a spontaneous labour.
Vaginal examinations are necessary:
- to assess the cervix before and during induction
- to determine the best method of induction
- to monitor progress.
Speak to your midwife about ways that we can make a vaginal examination as comfortable as possible.
Hospital stay
An induction may mean a longer stay in hospital compared to a spontaneous labour.
If you are admitted to the Antenatal ward for the first stage of the induction process, your overall hospital stay is likely to be longer.
If you are having an induction because labour has not started naturally after 41 weeks, you will be offered an 'Outpatient induction'. This can reduce your overall hospital stay. For more information about outpatient induction, you can read our information on The induction journey: your options. You can also attend our online Induction of Labour workshop (see below).
Hyperstimulation
Fewer than 5 in 100 women whose labour is induced with hormonal methods may experience 'hyperstimulation. This is when the uterus contracts more than is normal, which may affect the baby’s heart rate. Hyperstimulation can be treated with medication if needed. Close monitoring of your contractions and your baby’s heart rate allows the team to detect hyperstimulation and if the baby is affected.
Induction may be unsuccessful
For a small number of women, induction may not work. This means labour does not start or does not progress. If this happens, you will have a discussion with a doctor about the option of a Caesarean birth.
Alternatives
Some women will try alternative methods to help labour start naturally. There is limited evidence about these methods. They include being active, acupuncture and nipple stimulation.
If you are considering any other methods to try and start labour, we recommend speaking to your midwife first. Some may not be safe to try.
Some women may also consider planning a Caesarean birth instead of an induction. If you decide this is something you want to consider, we will offer you an appointment to discuss this with an obstetrician or a senior midwife.
Being active
In late pregnancy, being upright and moving may help your baby to settle into your pelvis and press on your cervix. There is some evidence that walking for 30 minutes, three times a week, may increase your chance of going into labour.
Being more active can also help you sleep and feel better. Listen to your body. Only walk as far and fast as is comfortable for you.
Acupuncture
There is little evidence to suggest that acupuncture can trigger labour. It may help the cervix to get ready for labour, but more research is needed. If you do want to try acupuncture, check that the practitioner is fully qualified, registered, and has experience providing it to pregnant women. They should always use disposable needles.
Nipple stimulation
There is a small amount of evidence to suggest that nipple stimulation may help labour start.
If you want to try it, we recommend waiting until you are at least 36 weeks pregnant. Gently rub or roll your nipples or try hand expressing. This releases oxytocin, which is the hormone that stimulates contractions.
Instinct
What do you feel is right for you? What feels safest? What does your gut instinct tell you?
Nothing
If you decide to do nothing your options are to continue waiting for labour to start naturally or to delay the date of your induction.
If you decide you do not want to be induced within the recommended time-frame, you will be offered an appointment with an obstetrician or senior midwife to make another plan. This plan may include the offer of additional monitoring to check your baby’s well-being and to see if the placenta is working normally.
It is important to understand that these checks offer a snapshot of how your baby is doing at that moment in time. They are not able to identify problems before they occur, and they do not prevent problems from happening.
Learn more about induction
There are several ways to induce labour. Which method is offered to you will depend on your and your baby's individual circumstances.
You can read more about the different methods in our information on The induction journey: your options.
You can also book onto our Induction of labour online workshop.
This one-hour session is for anyone booked for an induction at Kingston Maternity Unit. It is run by midwives. You can learn about:
- the process of induction
- the different methods that may be offered
- what to expect during your stay with us
- what to bring
- ways to make the experience a positive one.
Kingston Maternity Induction of labour online workshop
Thursdays, 10 to 11am
Book through Eventbrite
What next
You will be offered an appointment to discuss your options. You can change your mind at any point. You can watch one woman's account of her positive induction experience at Kingston here.
References
Muglu J et al. Risks of stillbirth and neonatal death with advancing gestation at term: A systematic review and meta-analysis of cohort studies of 15 million pregnancies. 2019 Jul 2; 16(7): e1002838.
Inducing labour. NICE guidance [NG207]. 04 November 2021
Contact information
Maternity helpline
Telephone:

