Neurodiversity information for parents and young people
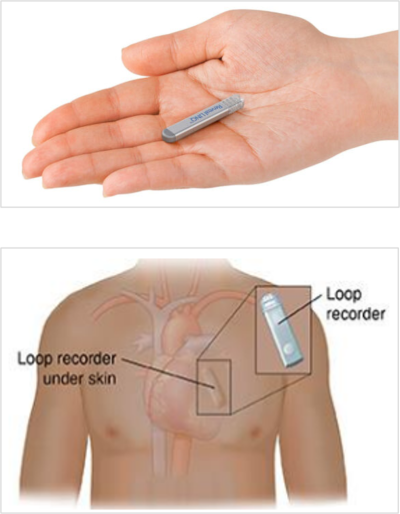
About implantable loop recorders (ILRs)
An ILR is a monitor which is implanted just under your skin on your chest wall. The ILR allows your heart’s electrical activity to be recorded. Your doctor or Clinical Nurse Specialist (CNS) can review the information to help diagnose and manage your condition.
How long you will have your ILR inserted
You may need the ILR for a few days, a few months, or possibly longer. It will depend on your condition and the information the ILR gives us. Your doctor or CNS will decide when it is safe to remove the ILR and discuss this with you.
How an ILR is fitted
The ILR is inserted under the skin on your chest. We give you a local anaesthetic. We make a small incision (cut) of about 2 centimetres to allow us to insert the device. The procedure typically takes 15 to 30 minutes.
Who performs your procedure
Most ILRs are implanted by a CNS trained by a cardiology consultant. Occasionally a doctor carries out the procedure.
Does the procedure hurt?
The injection of the local anaesthetic may sting and cause slight discomfort. You may feel a slight pressure when we insert the ILR.
Once the ILR is implanted, we will close the small incision with Steri-Strips.
Why you need an ILR
Your doctor or CNS may recommend an ILR if you have one or more of the following symptoms or health conditions.
| Symptom or condition | Why we monitor |
| Unexplained fainting: A transient (temporary) loss of consciousness, also known as ‘passing out’. This can occur for a number of reasons, including low blood pressure and abnormal heart rhythms. | Fainting can be serious if caused by an abnormal heart rhythm. |
| Heart palpitations: A usually harmless condition in which the heart feels as if it is pounding, racing or fluttering. | Palpitations may indicate a serious, underlying heartcondition. |
| Atrial fibrillation: A common condition when the upper chambers of the heart beat fast and irregularly. Also called AF or AFib. | AFib requires treatment because it is strongly linked to stroke. |
| Unexplained stroke: A stroke of unknown cause that may be triggered by AFib, causing a blood clot to form and block oxygen to the brain. | Detecting AFib after stroke may help healthcare professionals to prevent a second stroke. |
What happens at your pre-assessment appointment
We will give you a pre assessment appointment about 7 days before your procedure.
Your appointment letter will explain where you need to go. It is likely that we will give you an appointment for an ECG before you see the CNS.
Following this we will also give you a blood test and take some swabs. You will probably be in the hospital for around 1 hour.
During your pre assessment appointment, the CNS will explain what you should bring to hospital with you on the day of the procedure. They will also tell you how to prepare for the procedure, as follows:
- If you can, we recommend you have a shower before you come to the hospital.
- Wear comfortable, loose clothing to the hospital.
- Remove all jewellery and nail varnish before you arrive.
- You can bring your phone, spectacles, and hearing aids with you.
- Bring a dressing gown, slippers and your medicines.
If you take warfarin or Fragmin
If you take warfarin
Continue taking warfarin.
When you receive your appointment letter, contact the clinic or doctor who supervises your blood tests and let them know the date of your procedure. They may recommend an alternative form of anticoagulation drugs.
We will give you a blood test at the hospital on the day of your procedure.Bring your anticoagulant records with you to the hospital.
If you have Fragmin injections
Do not inject your dose on the morning of the procedure. This will reduce the possibility of excessive bleeding during or after the procedure.
If you take apixaban, dabigatran, edoxaban or rivaroxaban
Take your last dose at least 24 hours before your procedure.
On the day of your procedure
You can expect the following on the day of your procedure.
- We will ask you to remove your shirt or top and give you a hospital gown to change into.
- A nurse will go through pre admission checks with you.
- We will ask you to sign a consent form if you have not already done this.
- We will clean the area of your skin where we will insert the ILR.
- We will cover you in a blue sterile sheet with an opening over your chest. We will fold the sheet so that your face is not covered.
- We will inject you with a local anaesthetic on your chest where we plan to insert the ILR. The anaesthetic will take a few minutes to take effect. We will make a small incision and insert the ILR.
- We will monitor your heart during the procedure.
In rare cases where clotting levels have not returned to a safe limit, we will postpone the procedure to avoid medical complications.
Professional observers
The department where your procedure will take place regularly has professional observers present. Most of these observers are healthcare professionals who are qualified or in training. Occasionally they are specialist company representatives.
![]()
Tell a doctor or nurse if you do not wish observers to be present during your procedure.
Following your procedure
You can expect the following after the procedure.
- A member of the cardiology team will programme the ILR and ensure is it working properly. They will explain how you can use the ILR device and give you written information about how to use it.
- We will offer you a hot drink and a biscuit and keep an eye on you for 1 hour.
- The CNS will see you before you go home and discuss next steps in your care. They will give you a discharge summary that explains the ILR procedure, how to take your medicine(s) and follow up steps.
- We will send a copy of your discharge summary to your GP.
- Before you leave we will give you a date and time for a 6 week follow up check.
After care
You may feel some mild discomfort around the ILR insertion site, but once it has healed, most people do not notice the ILR. The steri strips used to close the wound will fall off after a few weeks. If this does not happen, visit your GP to have them removed.
Do not rub or massage your skin on the site of the ILR, because this can move the ILR and cause it to stop working.
Important
If the skin around the ILR becomes red, sore, more swollen, or inflamed, contact the the Cardiology Pacing Team (see Contacts section).
![]()
Go to your nearest ED (A&E) if you become unwell, develop a high temperature or notice changes to the skin around the ILR and cannot get hold of the Cardiology Pacing Team.
Benefits and risks of the procedure
The benefits of having an ILR fitted far outweigh risks of the procedure.
An ILR alerts the cardiac team to changes in your heart rhythm that may cause your symptoms. This allows us to provide prompt treatment for potentially serious conditions.
As with any kind of surgery, there are small risks associated with the procedure. These include:
- infection
- bleeding
- discomfort during the procedure.
On rare occasions, these factors may cause us to remove the ILR.
More information
Arrhythmia Alliance Information and advice for arrhythmia patients
British Heart Foundation general information
NHS information on having a pacemaker fitted
NHS information on TOE (transoesophageal echocardiogram)
Contact information
Kingston Hospital Cardiology Department Admin Team, Monday to Friday 9am to 5pm
or
Kingston Hospital Cardiac Nurse Specialists (CNS), Monday to Friday 9am to 5pm
or
Kingston Hospital Device Clinic, Monday to Friday 9am to 5pm
or
Kingston Hospital Cardiology Pacing team, Monday to Friday 9am to 5pm
Telephone:
Cardiology Dept Admin: 020 8934 2321 option 1
CNS: 020 8934 6453
Device Clinic: 020 8934 3854 or 020 8934 3104
Cardiology Pacing team: 020 8934 3872