Neurodiversity information for parents and young people
![]()
Take time to read this information as soon as you can.
It explains the tests and treatment options available at the hysteroscopy clinic and how you need to prepare. We will give you further explanations at your consultation and you will have an opportunity to ask questions.
On arrival, report to the reception desk in Gynaecology Procedure Outpatients.
Why we have referred you to this clinic
We may have referred you for one of the following reasons:
- Bleeding after the menopause (postmenopausal bleeding)
- Heavy periods
- Bleeding in between periods
- Irregular bleeding whilst on hormonal treatment
- Removal of a coil when the threads are not visible at the cervix
- Fertility concerns
- Following a miscarriage
- To investigate something seen inside the uterus on an ultrasound scan, such as an endometrial polyp or fibroid.
We have offered you this appointment so that we can find the cause of your problem and plan or undertake treatment, if needed.
Before your clinic appointment
If you have had sex recently
The hysteroscopy cannot go ahead if you have had sex without using contraception in the last month or since your last period.
![]()
If this is the case, phone the Clinic Pathway Coordinator to reschedule the appointment using the contact information below.
If you have vaginal bleeding
It is important that you still attend your appointment.
Sometimes it can be difficult to do a hysteroscopy if you are bleeding heavily, but other tests can still be done.
![]()
Ring the Clinic Pathway Coordinator using the contact details below if you have questions.
Confirm your appointment
Confirm that you will be attending the appointment by calling the Clinic Pathway Coordinator using the contact information below.
We recommend that you take pain relief at least 1 hour before your appointment. (400mg of ibuprofen or 1 gram of paracetamol or whichever pain relief you find useful for period pain).
Preparing for your appointment
- Eat and drink normally. You do not need to fast before your appointment.
- Take pain relief (see box above).
- Bring a list of any medications that you are taking with you.
- You may wish to have a friend or family member accompanying you.
At your appointment
A gynaecology healthcare professional will see you and discuss your gynaecological problem. Most women attending this clinic will have an investigation called a hysteroscopy (also known as an outpatient hysteroscopy or OPH). Other investigations and treatments may also take place and these are explained in this leaflet.
Your healthcare professional will discuss what will happen and ask for your consent. Please take this opportunity to ask any questions you may have.
A hysteroscopy cannot be performed if there is any chance that you are pregnant. We may offer you a urine pregnancy test on your arrival at your appointment.
You can expect to be in the outpatient department for approximately 1 hour.
Some women may be required to return for medical treatment, further investigations, or surgery. We will discuss this with you at your appointment.
The nature of gynaecological and obstetric care means that intimate examinations are often necessary. We understand that for some people, particularly those who may have anxiety or who have experienced trauma, physical or sexual abuse, such examinations can be very difficult.
If you feel uncomfortable, anxious or distressed at any time before, during, or after an examination, please let your healthcare professionals know. If you find this difficult to talk about, you may communicate your feelings in writing.
Your healthcare professionals are there to help and they can offer alternative options and support for you.
Remember that you can always ask them to stop at any time and a chaperone will be present. You can also bring a friend or relative.
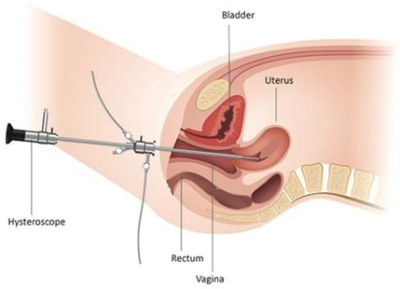
About hysteroscopy
A hysteroscopy is a procedure that involves examining the inside your uterus (womb). We do this by passing a thin telescope-like device called a hysteroscope, which is fitted with a small camera, through the neck of your womb (cervix).
The healthcare professional doing the procedure can then see whether there are any problems inside your uterus that may need further investigation or treatment.
There will be 2 or 3 healthcare professionals in the room and they will support you throughout the procedure.
They will ask you to change into a hospital gown.
They will help you to get into position in a special chair and will keep you as covered up as possible.
To perform a hysteroscopy, we pass a hysteroscope through your cervix to give us a clear view of the inside of your uterus. No cuts are needed. We pass fluid (saline solution) into your uterus to help us to see the inner lining and you will feel wet as the fluid trickles back out.
If we do not find any problems, the actual procedure will only take about 5 to 10 minutes. Sometimes, we may take a biopsy (small sample) from the lining of your uterus and send it to the laboratory for examination.
The biopsy can be painful, but the pain should not last long. If we find a polyp or fibroid, we can sometimes remove it at the same time by using additional instruments. We may offer you a local anaesthetic to make you more comfortable, particularly if a wider hysteroscope needs to be used. Tell your healthcare professional if the procedure is becoming painful.
During the procedure, your healthcare professional will look inside your uterus on a screen and you can also watch the screen if you choose to. We often take photographs of the findings inside your uterus and keep them in your healthcare notes.
How long does it take?
The hysteroscopy may only take 5 to 10 minutes. If you are having another procedure such as a small fibroid removed it may take longer.
The total visit will take up to one hour including consultation, having the procedure, and recovery.
You can rest in the outpatient clinic’s recovery area for as long as you need (usually about 20 minutes).
Treatment options that we might offer you at the same time as your hysteroscopy
Insertion of a Hormonal Intrauterine System (IUS) Mirena Coil
This is a T-shaped contraceptive device placed in your uterus (womb). It releases a small amount of progestogen and can help heavy periods.
Advantages
- Low dose of safe hormone
- Progesterone makes the lining of the womb thin which can result in lighter periods or periods stopping
- Studies show that it can help painful periods
- More than 99% effective as contraceptive
- Lasts for up to 5 years ('Fit it and forget it')
Disadvantages
- Possible irregular bleeding which takes a few months to settle
- Must be inserted by a clinician
Alternatives
- Non-hormonal medicines such as tranexamic and mefanamic acid
- Oral or injectable hormonal treatments.
Polyp removal
Polypectomy: a polyp inside the uterus is a skin tag that looks like a small grape, sometimes on a stalk. Polyps are formed as a result of overgrowth of the lining of the uterus. If not too big, polyps can sometimes be removed at the same time as the hysteroscopy.
Advantages
- Removal can sometimes stop irregular or heavy bleeding.
- If removed at the same time as the initial hysteroscopy, avoids a further procedure under a general anaesthetic.
Disadvantages
- Risks the same as for the hysteroscopy. Takes a little longer so may feel more cramping pain.
Alternatives
- Polyps can be left, although it is usually advisable to remove them as they can be the cause of bleeding problems.
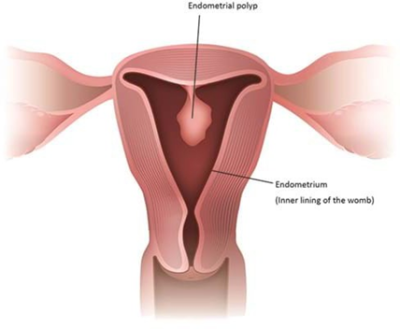
Removal (resection) of small fibroids affecting the inside of the uterus.
Fibroids are knots in the muscle of the uterus that are non-cancerous (benign). They can sometimes bulge like a polyp into the lining of your uterus and your healthcare professional may advise removal to help with your symptoms.
If not too big, sub mucous fibroids that grow into the cavity of the uterus can sometimes be removed at the same time as the hysteroscopy.
Advantages
- Removal can make heavy periods lighter.
- If removed at the same time as the initial hysteroscopy, avoids a further procedure under a general anaesthetic.
Disadvantages
- Risks the same as for the hysteroscopy. Takes a little longer so may feel more cramping pain.
Alternatives
- Fibroids can be left, although it is usually advisable to remove them. They can make periods heavier. We will advise you to have them removed if we think they are causing heavy bleeding.
Other
- Endometrial biopsy: taking a sample from the lining of the uterus. This can be done through the hysteroscope or after inserting a speculum and passing a thin tube through the cervix. You may experience severe period-like pain during this procedure, but the pain should not last long.
- Removal of a coil from the uterus when the threads are not visible.
For most women, a hysteroscopy is quick and safe, and is carried out with little pain or discomfort. It is normally done without inserting a speculum (a special tool made of metal or plastic), by using a thin telescope (called vaginoscopic OPH) as this is more comfortable. If other investigations or treatment are needed, a speculum may be used. Everyone’s experience of pain is different and some women will find the procedure painful.
If it is too painful for you, let your healthcare professional know as the procedure can be stopped at any time if you wish.
Your healthcare professional may offer you a local anaesthetic injection into your cervix. This will require using a speculum to see your cervix. Your healthcare professional will discuss this with you.
If you feel anxious about the procedure, talk to your healthcare professional about this when you arrive.
Alternatives to hysteroscopy
There may be other things to consider when deciding whether a hysteroscopy is the right choice for you, such as:
- If you faint during your periods because of pain.
- If you have experienced severe pain during a previous vaginal examination.
- If you have experienced difficult or painful cervical smears.
- If you have had any previous traumatic experience that might make the procedure difficult for you.
- If you do not wish to have this examination when awake.
You may choose to have your hysteroscopy with either a general or spinal anaesthetic. This will be done in an operating theatre, usually as a daycase procedure and not during this appointment. You can discuss this option with your healthcare professional when you come for your appointment. The risks and complications are lower when hysteroscopy is done as an outpatient procedure rather than under anaesthesia.
You may choose not to have a hysteroscopy at all, though this may make it more difficult for your healthcare professional to find the cause of your symptoms and to offer the right treatment for you. They may then recommend a scan and a biopsy to find out more information and/or may ask you to come back if your symptoms continue.
After your procedure
How you may feel afterwards
You may get some period-like pain for 1 to 2 days.
You may also have some spotting or fresh (bright red) bleeding. We will provide you with a pad, but you are welcome to bring your own pad if you wish to. The bleeding may last up to 1 week. We advise you to use pads rather than tampons for any bleeding in the two weeks following the procedure.
These symptoms usually settle very quickly. Most women feel able to go back to their normal activities on the same day.
- You can shower as normal.
- You can resume your normal physical activity and sex when any bleeding and discomfort has settled.
- If needed, you can take pain relief such as 400 mg of ibuprofen every 8 hours or 1 gram of paracetamol every 4 hours, or your usual period pain tablets.
Follow up after your procedure
Some women may not need a follow up appointment. We will send you and your GP a letter summarising what happened at your appointment including any results from tests, normally within 10 working days.
Your healthcare professional will discuss any further treatment needed with you. If any follow up appointments are needed, your health care professional will tell you about this and we will send you a letter with the appointment details within 7 days.
Symptoms to look out for after your procedure
- Abdominal pain that does not go away, even after taking painkillers.
- Heavy bleeding (for example, needing to change a pad more than every half hour and not easing after 2 to 3 hours).
- A temperature, smelly vaginal discharge, shivers and feeling generally unwell (these are all signs of an infection).
- If you experience any of these, seek advice from a health professional straight away. This could be your GP, a GP at a walk-in or urgent care centre, or go to your nearest Emergency Department (A&E).
Possible risks
The possible risks of a hysteroscopy and other investigations or treatments that might take place are:
- Pain during or after a hysteroscopy is usually mild and similar to period pain. Simple pain relief medications can help. On occasion, women may experience severe pain.
- Feeling or being sick or fainting can affect a small number of women. However, these symptoms usually settle quickly. Let your healthcare professional know if you are feeling unwell during or straight after the procedure.
- Bleeding is usually very mild and is lighter than a period, settling within a few days. We advise you to use pads (sanitary towels), not tampons. If the bleeding does not settle and gets worse, contact your GP or nearest emergency department (A&E).
- Infection is uncommon (1 in 400 women). It may appear as a smelly discharge, fever or severe pain in the tummy. If you develop any of these symptoms, contact your healthcare professional urgently.
- Failed/unsuccessful hysteroscopy occurs if it is not possible to pass the hysteroscope inside your uterus. Usually this happens when the cervix is tightly ‘closed’ or scarred. If this happens, your healthcare professional will discuss alternative options with you.
- Damage to the wall of the uterus (uterine perforation). Rarely, a small hole is accidentally made in the wall of the uterus. This could also cause damage to nearby tissues. This happens in fewer than 1 in 1000 diagnostic hysteroscopy procedures, but is slightly more common if someone has a polyp or fibroid removed at the same time. It may mean that you have to stay in hospital overnight. Usually, nothing more needs to be done, but you may need a further operation to repair the hole.
Contact information
Kingston Hospital Hysteroscopy Clinic, Gynaecology Outpatients Department (Willow Building)
Telephone:
Gynaecology Clinic Pathway Coordinator 020 8934 6407