Neurodiversity information for parents and young people
Read this information as soon as your doctor has recommended a colonoscopy. It covers what you need to know before having a colonoscopy. It includes essential information about the procedure and how to prepare for it. You may need to start preparing 7 days beforehand.

Key messages
1. Contact the nurse helpline now:
- if you are pregnant, or may be pregnant
- if you have a pacemaker
- if you have an implantable heart defibrillator
- if you take any medicine to help prevent clots, such as warfarin, rivaroxaban (Xarelto), apixaban (Eliquis), edoxaban (Lixiana) or dabigatran (Pradaxa)
- if you have a stoma.
2. Check the list of medicines to see if you need to change yours beforehand
Look at Medicines when having an endoscopy for details of which medicines must be stopped or changed beforehand.
3. Carefully read the bowel preparation instructions
Look at the instructions for bowel preparation we have also sent you. This must be started 3 to 7 days before the procedure. Your colonoscopy may not go ahead if you have not completed the bowel preparation as instructed.
4. If you have diabetes, check the separate instructions
Look at Diabetes and having an endoscopy if you have diabetes.
5. Plan how you will get home
During the procedure, you may have medicines to relax you and relieve pain. If so, you must arrange to have a responsible adult to take you home and stay with you for 24 hours. During this time, you will not be able to, for example, drive, use the oven or kettle, go back to work or look after small children.
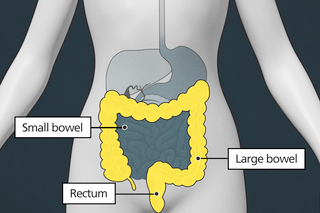
About a colonoscopy
Shared decision making and informed consent
Your healthcare team have suggested a colonoscopy. However, it is your decision to go ahead with the procedure or not. This document will give you information about the benefits and risks to help you make an informed decision.
Shared decision making happens when you decide on your treatment together with your healthcare team. Giving your ‘informed consent’’ means choosing to go ahead with the procedure having understood the benefits, risks, alternatives and what will happen if you decide not to have it. If you have any questions that this document does not answer, it is important to ask your healthcare team.
Once all your questions have been answered and you feel ready to go ahead with the procedure, you will be asked to sign the informed consent form. This is the final step in the decision-making process. However, you can still change your mind at any point.
Benefits
A colonoscopy is performed so that your healthcare team can find out why you are experiencing particular symptoms. The results will help them decide what treatment you may need.
Your symptoms may include:
- bleeding from your back passage
- diarrhoea
- small traces of blood in your faeces (poo)
- constipation
- unexplained weight loss
- you are anaemic (your body does not produce enough healthy red blood cells).
Another reason for a colonoscopy may be that you or members of your family have a history of inflammatory bowel diseases (ulcerative colitis or Crohn’s disease), bowel cancer or polyps. Polyps are extra growths of tissue on the bowel wall that can range in size. They are usually benign (not cancers), but if left can sometimes become cancerous.
If the endoscopist (the person doing the procedure) finds a problem, they can perform biopsies (removing small pieces of tissue) to help make the diagnosis. Sometimes a polyp is found and the endoscopist may be able to remove it during the procedure.
Alternatives
Your healthcare team have suggested a colonoscopy as it a good way to help diagnose the cause of the symptoms within your large bowel.
Other options include a CT colonography (a CT scan of your large bowel). If your doctor finds the cause of your symptoms, you may still need a colonoscopy to treat it or perform biopsies.
Another option may be a capsule endoscopy. This involves swallowing a tiny camera inside a pill that takes photographs of your large bowel.
If you decide not to have the procedure or the procedure is delayed
Your healthcare team may not be able to confirm what is causing your symptoms, and they may get worse. If they do, you should speak to your healthcare team.
If you decide not to have a colonoscopy, you should discuss this carefully with your healthcare team.
Before the procedure
Medicines
If you take warfarin, clopidogrel or other blood-thinning medication or are diabetic, let your healthcare team know at least 10 days before the procedure.
If you are diabetic, you will need special advice depending on the treatment you receive for your diabetes. Look at Diabetes and having an endoscopy with bowel preparation if you have diabetes.
If you take iron tablets, stop taking them at least 7 days before the procedure.
If you can, stop taking loperamide and codeine for 3 days before the procedure.
Look at Medicines when having an endoscopy for more details of which medicines must be stopped or changed before a colonoscopy.
Preparation
You will need to follow a special diet and should be given information about this before the procedure. You will be given strong laxatives to take before the procedure. This is to make sure your large bowel is empty so the endoscopist can have a clear view. Laxatives can make you dehydrated, so drink plenty of fluids before the procedure. If you cannot drink fluids, have severe abdominal pain or continuously vomit, speak to your healthcare team. You may have a higher risk of dehydration or too much fluid if you are already dehydrated, older or are taking large doses of diuretics (water tablets) for heart or kidney disease.
Laxatives can affect how well your body absorbs medication. Do not take medication orally (by mouth) within one hour of taking the laxatives. If you are unsure of anything, speak to your healthcare team.
When you arrive
We will be happy to answer any questions when you come in. Please ask if you wish to discuss anything in private.
The healthcare team will carry out a number of checks to make sure you have the procedure you came in for. You can help by confirming your name and the procedure you are having with your healthcare team.
The healthcare team will ask you to sign the consent form once you have read this document and they have answered your questions. You will be asked to confirm your consent on the day of the procedure.
What the procedure involves
A colonoscopy usually takes 30 to 45 minutes.
A cannula (thin, hollow tube) may be put in your arm or the back of your hand. This allows the endoscopist to give you medication during the procedure.
Some medications that may be used are:
- a sedative that will help you feel comfortable. You will be conscious and able to ask and answer questions, but you will feel relaxed
- pain relief that will reduce the chance of you experiencing severe pain or discomfort during the procedure
- medication to relax your muscles (Buscopan). This will make the procedure more comfortable. Buscopan can affect the pressure in your eyes so let the healthcare team know if you have glaucoma.
The endoscopist will ask you to lie on your left side to start with. You will be asked to move into different positions, such as lying on your back, to help the colonoscope move into the right position.
The healthcare team will monitor your oxygen levels and heart rate using a finger or ear clip. If you need oxygen, they will give it to you through a mask or small tube under your nostrils.
The endoscopist will place a flexible endoscope into your back passage. Air will be blown into your large bowel to help the endoscopist have a clear view.
The endoscopist will be able to look for what is causing your symptoms, such as inflammation. They may also be able to remove polyps. Most polyps can be removed painlessly and completely during the test. For larger polyps your endoscopist may only perform biopsies. Biopsies are taken using forceps (like tiny tongs) that are passed through the endoscope. You will be asked to come back to hospital to have the large polyps removed.
You may feel some discomfort during the procedure and your stomach may feel bloated because air is blown into your large bowel to help the endoscopist have a clear view.
Photographs and videos may be taken during the procedure. These may help with your treatment and are stored securely by your healthcare team and discussed with other healthcare professionals.
If you are awake during the procedure and at any time you want it to stop, let the endoscopist know. They will end the procedure as soon as it is safe to do so.
Can I be sent to sleep for the procedure?
In rare cases the procedure can be performed with you asleep under a general anaesthetic or deep sedation. If this an option for you, the healthcare team will talk to you about this before your procedure date.
General anaesthetic is given through the cannula, or as a mixture of anaesthetic gas that you breathe through a tube that passes into your airways. This means you will be unaware of the procedure.
A general anaesthetic has a higher risk of complications than other forms of medication. The healthcare team can give you more information about these. You may also need to wait longer for your procedure.
Most patients manage well without a general anaesthetic.
Complications
The healthcare team are trained to reduce the risk of complications.
Any risk rates given are taken from studies of people who have had this procedure. Your healthcare team may be able to tell you if the risk of a complication is higher or lower for you.
Possible complications of this procedure are shown below from most to least likely. Some can be serious. Rarely, you may need to come back into hospital for more treatment, including surgery.
![]()
| Common More than 1 in 20 |
Pain during and after the procedure Procedure not completed
We may recommend a repeat procedure or an alternative investigation. Bleeding from your bottom |
| Less common Up to 1 in 20 |
Complications of sedation
Missed abnormalities |
| Rare Up to 1 in 100 |
Dehydration Hole in bowel Significant bleeding
Heavy bleeding requiring blood transfusion and admission is very rare (around 1 in 2,400 cases). Injury to the spleen |
After the procedure
After the procedure you will be transferred to the recovery area where you can rest.
If you were not given a sedative, you should be able to go home after a member of the healthcare team has spoken to you and decided you are ready. If you were given a sedative, you will usually recover in about 1 hour, but this depends on how much sedative you were given. You may feel a bit bloated for a few hours, but this will pass.
The healthcare team will tell you what was found during the colonoscopy and discuss with you any treatment or follow-up you need. Results from biopsies will not be available until a later date so the healthcare team will write to you, call you or ask you to come back to the clinic to give you the results.
Before you leave, you will be given a discharge advice sheet and a copy of your colonoscopy report. The advice sheet will explain who to contact if you have any problems after your procedure. A copy of the report will be sent to your GP and doctor.

- if you go home the same day, a responsible adult should take you home in a car or taxi. They should stay with you for at least 24 hours unless your healthcare team tells you otherwise
- be near a telephone in case of an emergency
- do not drive, operate machinery or do any potentially dangerous activities (this includes cooking) for at least 24 hours and not until you have fully recovered feeling, movement and co-ordination
- do not sign legal documents or drink alcohol for at least 24 hours.
You should be able to return to work the next day unless you are told otherwise.
Once at home, if you experience pain or symptoms that are causing concern, contact the endoscopy unit, your GP or call 111. If you have serious symptoms, like severe pain or heavy bleeding, go to your nearest emergency department (A&E) straight away.
Summary
A colonoscopy is usually a safe and effective way of finding any problems with your large bowel. However, complications can happen. Being aware of them will help you make an informed decision about surgery. This will also help you and the healthcare team spot and treat any problems early.
Contact us
Endoscopy nurses helpline:
020 8934 6614 (2pm to 4pm only)
We strongly advise you read this information carefully before calling us. The answers to your questions may already be covered.
Call for questions relating to your procedure, medicines, or preparation for your test, which is not included in this leaflet and needs to be answered before you attend your appointment.
Make sure you have your hospital number ready before calling together with your full name and date of birth. Have a pen and paper ready too in case you need to write down information.
To reschedule or cancel appointments
Endoscopy Bookings: 020 8934 2099 option 2 (9am to 5pm) or Email khn-tr.
Your appointment is valuable. If you need to change your appointment, give us as much notice as possible, preferably at least 10 days. This allows us to offer the appointment to another patient.
Please note, the booking team cannot answer questions relating to the procedure.