Neurodiversity information for parents and young people
Read this information as soon as your doctor has recommended a gastroscopy. It covers what you need to know beforehand. It includes essential information about the procedure and how to prepare for it. You may need to start preparing 14 days beforehand.

Key messages
1. Contact the nurse helpline now:
- if you are pregnant, or may be pregnant
- if you have a pacemaker
- if you have an implantable heart defibrillator
- if you take any medicine to help prevent clots, such as warfarin, rivaroxaban (Xarelto), apixaban (Eliquis), edoxaban (Lixiana) or dabigatran (Pradaxa)
- if you have a stoma.
2. Check the list of medicines
Look at ‘Stop certain medicines’ (below) for details of which medicines must be stopped or changed beforehand.
3. Carefully read the stomach preparation instructions
Look at the instructions for stomach preparation (below). This must be started 6 hours before the procedure. Your gastroscopy may not go ahead if you have not followed the instructions to empty your stomach.
4. If you have diabetes, check the separate instructions
Look at Diabetes and having an endoscopy if you have diabetes.
5. Plan how you will get home
During the procedure, you may have medicines to relax you and relieve pain. If so, you must arrange to have a responsible adult to take you home and stay with you for 24 hours. During this time, you will not be able to, for example, drive, use the oven or kettle, go back to work or look after small children.
About a gastroscopy
Shared decision making and informed consent
Your healthcare team have suggested a gastroscopy. However, it is your decision to go ahead with the procedure or not. This document will give you information about the benefits and risks to help you make an informed decision.
Shared decision making happens when you decide on your treatment together with your healthcare team. Giving your ‘informed consent’’ means choosing to go ahead with the procedure having understood the benefits, risks, alternatives and what will happen if you decide not to have it. If you have any questions that this document does not answer, it is important to ask your healthcare team.
Once all your questions have been answered and you feel ready to go ahead with the procedure, you will be asked to sign the informed consent form. This is the final step in the decision-making process. However, you can still change your mind at any point.
Benefits
A gastroscopy is performed so that your healthcare team can find out why you are experiencing particular symptoms. The results will help them decide what treatment you may need.
Your symptoms may include:
- feeling sick
- vomiting
- abdominal pain
- difficulty swallowing
- bloating
- diarrhoea
- unexplained weight loss.
Another reason for a gastroscopy may be that you do not have symptoms , but you are anaemic (your body does not produce enough healthy red blood cells).
If the endoscopist (the person doing the procedure) finds a problem, they can perform biopsies (removing small pieces of tissue) to help make the diagnosis.
Alternatives
Your doctor has recommended a gastroscopy, with the camera being passed through your mouth. They think it is the best way of diagnosing most problems with your upper digestive system.
Alternative options could include having the gastroscopy camera passed through your nose.
A barium meal is an x-ray test of your upper digestive system. This test is not as accurate as a gastroscopy , and if your doctor finds a problem you may still need a gastroscopy to perform biopsies.
A urea breath test can be used to detect a germ (Helicobacter pylori) that can cause stomach ulcers.
If you decide not to have the procedure or the procedure is delayed
Your healthcare team may not be able to confirm what is causing your symptoms, and they may get worse. If they do, you should speak to your healthcare team.
If you decide not to have a gastroscopy, you should discuss this carefully with your healthcare team.
Preparing for your gastroscopy
Stop certain medicines up to 14 days before
There are certain medicines you must stop up to 2 weeks before your appointment. These are set out in the table below. You will be told when to restart these medicines before you go home after the gastroscopy.
Continue to take your other medicines as usual, unless the doctor or nurse tells you otherwise.
| Certain medicines for stomach acid | |
| omeprazole lansoprazole esomeprazole pantoprazole rabeprazole |
Stop these 14 days before the procedure. You will be told after the procedure when to restart these. Some people find it uncomfortable to stop these medicines but it is important. Otherwise we may not be able to spot certain problems during the gastroscopy. You can take antacids such as Rennies and Gaviscon. You can buy these, or cheaper unbranded versions, without a prescription. Do not stop these: If you have been given the gastroscopy appointment at short notice and there is less that 14 days to go, stop these stomach acid medicines as soon as you can. |
| Certain medicines to reduce blood clots (anti-coagulants and anti-platelets) | |
| pixaban clopidogrel dabigatran edoxaban prasugrel rivaroxaban ticagrelor |
You may need to stop these before your endoscopy. Do not stop without advice from an endoscopy or anticoagulant nurse, your hospital doctor or GP. Contact the endoscopy nurse helpline if you have not been given advice about these medicines |
| Warfarin | |
| warfarin |
You must speak to a nurse in the anticoagulation clinic at least 7 days before your gastroscopy. You may need to stop warfarin before your appointment, but do not stop it without medical advice. If necessary, you will be referred to the anti-coagulation clinic at Kingston Hospital. They will make the necessary arrangements for you. If you have not heard from them 7 days before your gastroscopy, contact them on 020 8934 2030, 020 8934 2041, 020 8934 3689 or 020 8934 2321, option 5. Stopping warfarin for a few days may slightly increase your risk of a clot. You can discuss this with the anticoagulation nurse on 020 8934 3576. If you take warfarin, we will check your INR with a finger prick test before your procedure. |
Other medicines
- On the day of the gastroscopy, take any regular medicines with a sip of water, unless you have been told not to take them. Do this 2 hours or more before your appointment.
- Bring a list of your current medicines with you when you come for the endoscopy.
- If you might need medicines such as asthma inhalers, insulin or angina sprays, it is important you bring these in too.
Emptying your stomach
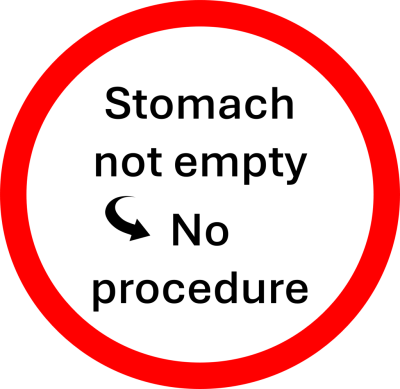
These instructions are very important. Your gastroscopy may not go ahead if you have not followed them.
|
|
6 hours before the appointment
|
|
|
4 hours before
|
|
|
2 hours before
|
Contact
Contact us on the nurse helpline if you have any questions
Diabetes
If you have diabetes, you may need to adjust your treatment whilst preparing for this procedure.
Look at Diabetes and having an endoscopy if you have diabetes:
- Discuss this with your GP or diabetes nurse specialist at least 3 days before your test.
- If you are on insulin, you should have an early morning appointment for the procedure. If you have been given a later appointment, contact the booking team to re-schedule. Adjust your insulin dose as necessary before your procedure.
When you arrive
We will be happy to answer any questions when you come in. Please ask if you wish to discuss anything in private.
The healthcare team will carry out a number of checks to make sure you have the procedure you came in for. You can help by confirming your name and the procedure you are having with your healthcare team.
The healthcare team will ask you to sign the consent form once you have read this document and they have answered your questions. You will be asked to confirm your consent on the day of the procedure.
What the procedure involves
A gastroscopy usually takes 10 minutes.
A cannula (thin, hollow tube) may be put in your arm or the back of your hand. This allows the endoscopist to give you medication during the procedure.
Some medications that may be used are:
- a throat spray with some local anaesthetic. This can taste unpleasant but helps to keep you comfortable during the procedure
- a sedative that will help you feel comfortable. You will be conscious so if at any time you want to procedure to stop, raise your hand. The endoscopist will end the procedure as soon as it is safe to do so
- pain relief that will reduce the chance of you experiencing severe pain or discomfort during the procedure
- medication to relax your muscles (Buscopan). This will make the procedure more comfortable. Buscopan can affect the pressure in your eyes so let the healthcare team know if you have glaucoma.
You will be asked to remove any false teeth or plates. The endoscopist will ask you to lie on your left side and a plastic mouthpiece will be placed in your mouth. This will keep your mouth open and stop you biting the endoscope.
The healthcare team will monitor your oxygen levels and heart rate using a finger or ear clip. If you need oxygen, they will give it to you through a small tube under your nostrils.
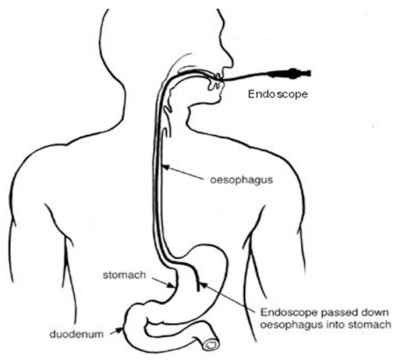
The endoscopist will place an endoscope into the back of your throat. They may ask you to swallow when the endoscope is in your throat. This will help it to pass easily into your oesophagus and down into your stomach. From here the endoscope will pass into your duodenum.
You may feel some discomfort during the procedure and your stomach may feel bloated because air is blown into it to help the endoscopist have a clear view. The endoscopist will be able to look for problems such as inflammation or ulcers and perform biopsies. Biopsies are taken using tiny forceps that are passed through the endoscope.
Photographs and videos may be taken during the procedure. These may help with your treatment and are stored securely by your healthcare team and discussed with other healthcare professionals.
If at any time you want the procedure to stop, raise your hand to let the endoscopist know. They will end the procedure as soon as it is safe to do so.
Can I be sent to sleep for the procedure?
In rare cases the procedure can be performed with you asleep under a general anaesthetic or deep sedation. If this an option for you, the healthcare team will talk to you about this before your procedure date.
General anaesthetic is given through the cannula, or as a mixture of anaesthetic gas that you breathe through a tube that passes into your airways. This means you will be unaware of the procedure.
A general anaesthetic has a higher risk of complications than other forms of medication. The healthcare team can give you more information about these. You may also need to wait longer for your procedure.
Most patients manage well without a general anaesthetic.
Complications
The healthcare team are trained to reduce the risk of complications.
Any risk rates given are taken from studies of people who have had this procedure. Your healthcare team may be able to tell you if the risk of a complication is higher or lower for you.
Possible complications of this procedure are shown below from most to least likely to happen. Some can be serious. Rarely, you may need to come back into hospital for more treatment, including surgery.
![]()
| Common More than 1 in 20 |
Pain Sore or dry throat Procedure not completed |
| Less common Up to 1 in 20 |
Complications of sedation Damage to teeth, lips or gums Vomiting blood Further investigation or procedure |
| Rare Up to 1 in 100 |
Significant bleeding Missed abnormalities Lung infection Tear in the stomach, bowel or oesophagus |
After the procedure
After the procedure you will be transferred to the recovery area where you can rest.
If you were not given a sedative, you should be able to go home after a member of the healthcare team has spoken to you and decided you are ready.
If you were given a sedative, you will usually recover in about 1 hour, but this depends on how much sedative you were given. Once you are able to swallow properly, you will be given a drink. You may feel a bit bloated for a few hours, but this will pass.
The healthcare team will tell you what was found during the gastroscopy and discuss with you any treatment or follow-up you need. Results from biopsies will not be available until a later date so the healthcare team will write to you, call you or ask you to come back to the clinic to give you the results.
Before you leave, you will be given a discharge advice sheet and a copy of your gastroscopy report. The advice sheet will explain who to contact if you have any problems after your procedure. A copy of the report will be sent to your GP and doctor.

- if you go home the same day, a responsible adult should take you home in a car or taxi. They should stay with you for at least 24 hours unless your healthcare team tells you otherwise
- be near a telephone in case of an emergency
- do not drive, operate machinery or do any potentially dangerous activities (this includes cooking) for at least 24 hours and not until you have fully recovered feeling, movement and co-ordination
-
do not sign legal documents or drink alcohol for at least 24 hours.
You should be able to return to work the next day unless you are told otherwise.
Once at home, if you experience pain or symptoms that are causing concern, contact the endoscopy unit, your GP or call 111. If you have serious symptoms, like severe pain or heavy bleeding, go to your nearest emergency department (A&E) straight away.
Summary
A gastroscopy is usually a safe and effective way of finding out if there is a problem with the upper part of your digestive system. However, complications can happen. Being aware of them will help you make an informed decision about surgery. This will also help you and the healthcare team to identify and treat any problems early.
Contact us
Endoscopy nurses helpline:
020 8934 6614 (2pm to 4pm only)
We strongly advise you read this information carefully before calling us. The answers to your questions may already be covered.
Call for questions relating to your procedure, medicines, or preparation for your test, which is not included in this leaflet and needs to be answered before you attend your appointment.
Make sure you have your hospital number ready before calling together with your full name and date of birth. Have a pen and paper ready too in case you need to write down information.
To reschedule or cancel appointments
Endoscopy Bookings: 020 8934 2099 option 2 (9am to 5pm) or Email khn-tr.
Your appointment is valuable. If you need to change your appointment, give us as much notice as possible, preferably at least 10 days. This allows us to offer the appointment to another patient.
Please note, the booking team cannot answer questions relating to the procedure.