Neurodiversity information for parents and young people
This leaflet is for patients who have been asked to come to hospital for an ERCP procedure. This means Endoscopic Retrograde Cholangiopancreatography.
Important information about your visit
- Please read this leaflet before you arrive.
- We will be happy to answer any questions when you come for your appointment.
- Please allow up to 6 hours in total for your visit.
- We will try to see you as close to your appointment time as possible. If there are going to be any delays, we will let you know as quickly as possible.
- The procedure will be performed by or under the supervision of a Consultant Gastroenterologist.
Important
Contact the Endoscopy Unit (details given below) before you come for your ERCP appointment if:
- you may be pregnant
- you have an implanted cardiac pacemaker or defibrillator
- you are taking anticoagulant or antiplatelet medicines (Warfarin, Rivaroxaban, Apixaban, Edoxaban, Dabigatran, Clopidogrel, Prasugrel)
- you had previous stomach and/or pancreas surgery or you have a stoma.
About an ERCP
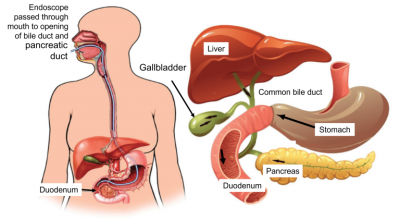
ERCP is an endoscopic (inside your body) procedure that helps doctors to diagnose and treat disorders of the biliary ducts, pancreatic ducts and pancreas.
A doctor steers a flexible tube (endoscope), which is about as wide as a finger, through your mouth and down your oesophagus (the food pipe that connects your mouth to your stomach), through your stomach and into your duodenum (part of your intestine which can also be called the top part of your small bowel). You can see the tube on the diagram below.
There is a light and a tiny camera on the end of the endoscope. The doctor then inserts a catheter (a tube less than two millimetres wide) through the endoscope to your bile duct (a tube or duct in the wall of your duodenum which bile and pancreatic juice pass through).
We then inject an X-ray dye into these ducts which allows the doctor to find any abnormalities, such as gallstones or strictures (narrowing of your tubes or ducts).
As well as finding abnormalities, we also use ERCP to do some therapeutic procedures including taking samples (biopsies), inserting tubes (stents) to relieve a blockage, or removing gallstones.
We can also use ERCP for other techniques, such as cholangioscopy. This is when a doctor passes a cholangiascope (mini-scope) through the ERCP to do a detailed assessment of ducts in your liver and pancreas.
General risks of any endoscopy procedure
- Damage to your teeth or dental work
- Discomfort in your upper abdomen (stomach area), bloating, belching (burping), retching and gagging
- A chest infection or pneumonia caused by aspiration of gastric fluids (accidentally breathing in fluids from your digestive system)
- Perforation: a hole or tear in the wall of the gullet (throat), stomach or duodenum. This occurs in approximately 4 in every 5,000 patients
- Bleeding following a biopsy. This occurs in approximately 1 in every 5,000 patients
- Allergy to intravenous sedation (a sedative drug injected into your vein to make you sleepy)
- Breathing, heart rate or blood pressure issues due to intravenous sedation. If this happens, we use other intravenous medicine to reverse the action of the sedative
- An abnormality being missed.
Specific risks of an ERCP procedure
- Inflammation of the pancreas (pancreatitis). This occurs in approximately 1 in every 30 patients.
- Measures are taken to reduce the risk of pancreatitis (e.g. an anti-inflammatory suppository). We will discuss this with you during the consent process. Pancreatitis is unpleasant and may require a longer stay in hospital, and on rare occasions it can be fatal.
- Infection within the bile ducts (cholangitis). This occurs in approximately 1 in every 200 patients.
- This usually settles down by itself, but it may require a longer stay in hospital and may require urgent treatment with antibiotics. Very occasionally, surgery is required.
- Infection of the gallbladder (cholecystitis). This occurs in approximately 1 in every 200 patients.
- Bleeding following a sphincterotomy (a cut at the lower end of the bile duct). This occurs in approximately 1 in every 200 patients.
A Consultant Endoscopist will discuss these risks with you before the procedure. Generally, the risk of having a complication is between 5 in 100 and 10 in 100 patients.
Statistically, the chance of dying within 30 days of having an ERCP is about 1 in 200 (0.5% of patients), but most of these deaths are the result of a serious underlying medical problem and not the procedure itself.
Sometimes an ERCP procedure cannot be completed because a gallstone or stricture (narrowing of a tube) makes access difficult or impossible. If this occurs, we may suggest a radiological procedure to relieve the blockage or transfer you to a tertiary centre (a healthcare centre with specific expertise in one area of medicine).
What to do before the ERCP
Blood Tests
You will need to have blood tests a few days before or as close to the procedure date as possible. These should include tests called bleeding parameters, full blood count, and liver and kidney function tests.
Book blood test
Please book your hospital blood test either:
- by phone on 020 3870 5766
- via our online platform ‘Sangix’.
Diabetes
- If you have diabetes, you may need to adjust your treatment whilst preparing for this test. Please discuss this with your GP or diabetes nurse specialist at least 3 days before your test.
- If you take Insulin, you should have an early morning appointment for your ERCP. If you are given an appointment at another time of day, please contact the booking team to re-schedule (number in Contacts section below).
- Adjust your Insulin dosage as appropriate before your ERCP procedure.
- Look at Diabetes and having an endoscopy.
Medication
- Bring a list of your current prescribed medication.
-
If you use asthma inhalers or angina sprays, it is important to bring these with you.
-
Follow the instructions in the table below.
| Medication | Action |
|---|---|
| Anti-coagulant or anti-platelets (such as clopidogrel, dabigatran, rivaroxaban apixaban, edoxaban, clopidogrel, ticagrelor or prasugrel) | Do not stop without medical advice. Your consultant will give you advice about these medications in clinic. Interrupting your anticoagulation medicines may carry a slightly increased risk of a blood clot forming. You can discuss this with the Anticoagulation Nurse (Contacts section below). |
| Warfarin |
Do not stop without medical advice. We will refer you to the Anticoagulation Clinic and they will contact you at least 7 days before your ERCP date. If they do not contact you, please call them (numbers are in the Contacts section below). We will check your INR (international normalised ratio) with a finger prick test before your procedure to check if you have a blood clotting problem. |
| Epilepsy | Do not stop taking your medication, but please be aware there may be a reduced effect and therefore a higher risk of an epileptic seizure. |
| Parkinson’s disease | Do not stop without medical advice. |
| Other regular medications not mentioned above | Take these as normal with a sip of water 4 hours before the procedure, unless advised not to by a health professional. |
![]()
Eating and drinking beforehand
| Time | What you can eat or drink |
|---|---|
| 6 hours before your procedure | You may have a light meal or food. You may drink as normal. |
| 4 hours before your procedure | No more food or drinks. You may have small sips of water, if needed. |
When you arrive at hospital
This is what will happen before your procedure.
- A nurse will check your personal details, blood pressure and pulse.
- A nurse or assistant will ask you to remove any spectacles, contact lenses or dentures just before the procedure (it is a good idea to leave jewellery and valuables at home).
- A nurse or assistant will ask you to change into a hospital gown.
- A nurse will insert a cannula (thin tube) into a vein on your arm so that we can give you intravenous medication.
- The Endoscopist who will carry out the procedure will discuss everything with you, answer any questions you may have, and then will ask you to sign the legal consent form.
Consent
We will involve you in all the decisions about your care and treatment.
If you decide to go ahead with the procedure and/or treatment, by law we must ask for your consent and we will ask you to sign a consent form. This confirms that you agree to have the procedure and you understand the risks and what it involves.
The Endoscopist will explain all the risks, benefits and alternatives before they ask you to sign the consent form. This leaflet is to help you make an informed decision about agreeing to the procedure. If you are unsure about anything, do not hesitate to ask to speak to a senior member of staff at any time during your appointment.
Anaesthetic and pain relief
The discomfort experienced during this procedure varies greatly from person to person.
You will be sedated during the procedure. A nurse remains with you throughout.
- A local anaesthetic throat spray will numb the back of your throat and numb the nerve-endings that cause gagging. It helps to reduce the sensation of the endoscope in your throat although it does not take away all the feeling and you may still gag a little.
- We will give you intravenous sedation (midazolam) and other medications via the cannula (thin tube) in your vein. The sedative will make you feel relaxed and drowsy.
- Intravenous pain killer (fentanyl) works with the sedative to make you more relaxed.
Instructions following sedation and pain killers
After the procedure you will need to do the following:
- You may need to rest on the ward for up to 4 hours to recover.
- You must arrange to have a responsible adult (escort) to take you home and stay with you for 24 hours. You will not be allowed to travel by public transport or travel alone in a taxi.
- Your escort will be contacted approximately 30 minutes before the time of discharge.
- For 24 hours after the sedative, you cannot return to normal activities such as driving, returning to work, operating machinery (including cookers and kettles), drinking alcohol, or signing legal documents.
- For 24 hours after the sedative, you cannot be responsible for small children.
Important after sedation
After sedation and pain killers, it is very important
you do the following:
- You may need to rest on the ward for up to 4 hours to recover.
- You must arrange to have a responsible adult (escort) to take you home and stay with you for 24 hours. You will not be allowed to travel by public transport or travel alone in a taxi.
- Your escort will be contacted approximately 30 minutes before the time of discharge.
- For 24 hours after the sedative, you cannot return to normal activities such as driving, returning to work, operating machinery (including cookers and kettles), drinking alcohol, or signing legal documents.
- For 24 hours after the sedative, you cannot be responsible for small children.
During the procedure
We will try to make the procedure as comfortable as possible for you.
- We will monitor your blood pressure, heart rate and oxygen level throughout.
- We will give you oxygen via a small sponge in your nostril or a nasal cannula (thin tube in your nose).
- We will give you a local anaesthetic throat spray to numb the back of your throat and medications to relax you, as explained above.
- We will ask you to lie on an X-Ray table and you will be exposed to radiation during the procedure.
- We will ask you to lie on your left side, with your left arm at the back and your right arm under the pillow.
- We will give you a small plastic mouth guard to bite on to protect your teeth. The Endoscopist will insert the endoscope through this into your mouth and down into your stomach and duodenum. This is not painful and will not make breathing or swallowing difficult, but it may feel uncomfortable and unpleasant.
- We will pass air into your stomach which may make you feel bloated. Most of the air is removed from your stomach at the end of the procedure.
- We will do a thorough assessment of your biliary system that includes your gall bladder, liver, and pancreas and also their ducts or passages.
- We may give you a non-steroidal anti-inflammatory suppository (via your rectum or bottom) to reduce the risk of pancreatitis (a type of infection).
- We may give you intra-venous antibiotics if you have a high risk of infection.
- If needed, we will take biopsies (small samples of tissue) and other specimens during the procedure (this is painless) and send these to the laboratory for testing.
- We may take photographs for your hospital records.
- Apart from the biopsies and specimens, the Endoscopist may take other types of sample, such as “brushings” for Cytology (a way to find a particular type of cell or organism).
- The ERCP procedure usually takes up to an hour, but it may be longer if we need to carry out more complex treatment procedures.
Afterwards
This is what happens after the ERCP.
- You must not eat or drink anything by mouth for 2 hours after the procedure.
- You will stay in the recovery area for up to 4 hours so that we can monitor you.
- You may have a mild sore throat, but this is nothing to worry about and will pass.
- You may feel bloated due to some air being left in your stomach, but this will pass out naturally.
- We will ask you to wait for the copy of your report and for a nurse to explain your discharge instructions to you.
![]()
When to call the Endoscopy Unit
![]()
Before you call, make sure you have your hospital number, full name and date of birth ready. Have a pen and paper ready in case you need to write down any information.
Rescheduling your appointment
![]()
Please note that the bookings team cannot answer clinical questions.
Give as much notice as possible, preferably at least 10 days’ notice. This will give us time to offer your appointment to another patient.
Contacts
| Endoscopy unit | 020 8934 6614 (2pm to 4pm) |
| Anticoagulation nurse | 020 8934 3576 |
| Anticoagulation clinic | |
| Endoscopy Bookings Team (reschedule or cancel appointments) |
020 8934 2099 |