Neurodiversity information for parents and young people
About eczema
Eczema is inflammation of the skin which can make it red, dry and flaky. Itching is the main symptom and children often scratch their skin, damaging it even more.
There is no single cause of eczema. Some family history factors make children more likely to have conditions such as eczema, asthma, hay fever and food allergies. If there is a family history factor, things like using soap, getting too hot, wearing wool or having contact with dust can trigger eczema. Stress, being unwell, and infections can also trigger eczema.
Eczema cannot be cured, but we can control it and prevent flare ups. Around 60 to 70% of children who have eczema in the first few years of their life will grow out of it by the age of 11.
What to use at home to help control your child's eczema
Use skin barrier emollients (moisturisers). Emollient treatments have an important role in treating eczema. They protect the skin from irritants and allergens and prevent loss of water from the skin. Ask your pharmacy for advice on choosing an emollient if you are unsure.
- Use an emollient regularly throughout the year, even when your child’s eczema is mild.
- Apply it on your child’s skin 4 to 6 times a day. Do this in one motion, following the direction of the hair. This will stop hair follicles from getting blocked.
- If you use an emollient with another topical product at the same time of day, apply one product at a time and then wait several minutes before applying the next product. You can choose which product you apply first. (A topical product is one that is applied to the skin).
- Aim to use up to a 500g tub or tube of emollient per fortnight.
- If your child finds the emollient uncomfortable or irritating, you can try a different brand.
- Use a leave-on emollient or an emollient soap substitute to wash your child’s skin, instead of soaps and detergent-based wash products. You can add leave-on emollients to bath water.
- If your child is under 12 months, use leave-on emollients or emollient soap substitutes instead of shampoos.
- For children older than 12 months, use an unperfumed brand and ideally one labelled as suitable for eczema.
- Avoid washing your child’s hair in bath water.
Treatments your GP can prescribe
Use the drop-down menu for information on treatments that your GP can prescribe to help your child's eczema.
Topical steroids
Topical steroids which are applied to the skin can help to reduce inflammation such as swelling, redness and itching during flare-ups of eczema.
Steroid ointments are not bad for the skin. The misconception that topical steroids always give side effects dates back to misuse of stronger steroid creams in the 1960s/70s. Long term continuous use can result in thinning of the skin. However the skin usually recovers when the cream is stopped, and this side effect is unlikely to happen now because steroids are usually prescribed to control flare ups and are not recommended for continuous use.
- Use steroid ointments or creams alongside skin barrier emollients.
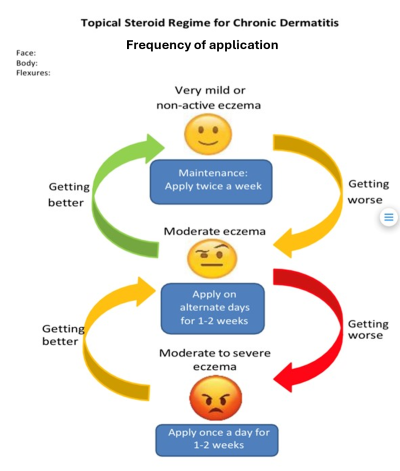
- Apply the ointment or cream daily when the skin is inflamed and then reduce the dose to alternate days for 1 or 2 weeks.
- When the eczema is no longer inflamed, the steroid ointment can be used twice a week (for guidance, use the diagram below).
Calcineurin inhibitors
These ointments can be used when steroid creams have not kept your child’s eczema well controlled. Two types are available, and they are particularly suitable for delicate areas of skin, for example the face.
- Tacrolimus (brand name Protopic) is used for moderate to severe eczema. Pimecrolimus (brand name Elidel) is used for mild to moderate eczema.
- They can sting when first applied so store them in the fridge before using them.
- We advise you to apply them in the evening.
- When using calcineurin inhibitors, it is important to avoid direct sunlight. Make sure your child is wearing factor 50+ sunscreen if they go out in the sun.
Other ways to help your child at home
You can do the following at home to help your child with eczema.
- Do an extra rinse when washing their clothes.
- Keep their fingernails short to prevent damage if they scratch their skin.
- Instead of allowing them to scratch the skin, apply a cold pack. Then gently pat the skin or blow cold air on the itchy area.
- Pat the skin dry after bathing them. Apply moisturiser to the eczema area straight afterwards.
- Remember to keep your GP up to date with the list of creams and/or ointments so you can order via repeat prescription.
Contact information
Dermatology Department, Kingston Hospital (Monday to Friday 9.00am to 5.00pm)
Telephone: