Neurodiversity information for parents and young people
This document is called a decision-aid. It will help you decide between different options for the birth of your baby. It is for women who have already had one caesarean birth.
We recommend you go through it and then talk to your midwife or obstetrician to make a decision together. You might also want to write down and talk about your thoughts about your previous birth so we know what matters to you.
At Kingston we are committed to supporting your choices for your birth.
Your options
If you have previously had a caesarean, it does not mean that this is your only option for future births. You can plan either:
- vaginal birth after a caesarean (VBAC)
- planned caesarean.
Planning a vaginal birth or another caesarean are generally safe choices.
Most women who have previously had one caesarean and then plan a vaginal birth with a future baby, do go on to have a vaginal birth.
Factors that might affect your decision
When deciding on whether to choose a vaginal birth or another caesarean, we recommend you consider the following.
- The benefits and risks of either option.
- How likely you are to be able to have a vaginal birth.
- What happened when you previously had a caesarean:
- why you had a caesarean
- the type of cut that was made in your womb (uterus) during the operation
- whether you had any complications at the time or during your recovery.
- Whether you have had a previous vaginal birth.
- How you felt about any previous births.
- Whether your current pregnancy is straightforward.
- How many more babies you are hoping to have in the future.
What is important to you for this birth
When deciding what type of birth you want, you might want to consider what is important to you. Talk through your preferences with your midwife. Consider, for example:
- the birth environment
- pain relief options
- support during and after the birth.
Possible benefits of each option
To help decide what option is best for you, you may want to consider the possible benefits of each type of birth.
Vaginal birth after caesarean (VBAC) |
Planned caesarean |
|
The possible benefits of VBAC include: a faster return to normal activities, with less pain and a lower chance of infection |
The possible benefits of a planned caesarean include: fewer anxieties about labour or birth |
If you plan a VBAC, what are the chances of a vaginal birth?
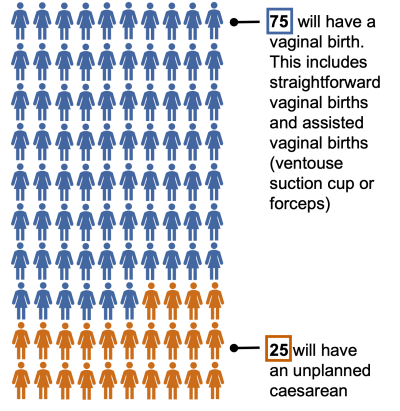
Most women who have previously had one caesarean and then plan a vaginal birth (VBAC) with a future baby, do go on to have a vaginal birth. This is usually straightforward but may sometimes result in an assisted vaginal birth. This is when a doctor helps the baby to be born with the assistance of a ventouse suction cup or forceps.
|
Out of 100 women choosing VBAC, with a straightforward pregnancy who go into labour naturally, how many have a vaginal birth? |
|
|
In 2021-22 at Kingston, 78 out of 100 women planning VBAC had a vaginal birth. |
|
|
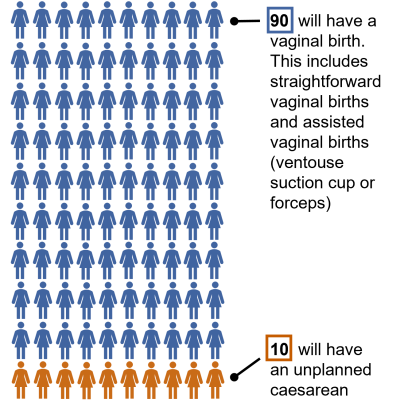
If a woman has also previously had a vaginal birth, the numbers are even higher:
|
|
Your chance of having a VBAC increases if:
- you go into labour naturally
- you have given birth vaginally before
- your baby is expected to be less than 4kg (8.8lbs)
- your previous caesarean was because baby was breech
- your previous caesarean was due to concerns about your baby’s heart rate
- you go into labour by 40 weeks
- you are less than 40 years old
- you are not obese.
If you plan a VBAC, where will you have your baby?
We recommend all women planning a VBAC give birth in our Delivery Suite (Labour Ward). Your baby’s heartbeat can be monitored continuously during labour to ensure their wellbeing. Changes in their heartbeat can be an early sign of problems with your previous caesarean scar. If a caesarean is recommended during labour, there is easy access to an operating theatre and the medical team.
Some women prefer to plan to give birth in our midwife-led unit (the “Birth Centre”) or at home. The baby’s heartbeat is monitored at regular intervals during labour. If this is your choice, we recommend an appointment with our Consultant Midwife to discuss this in more detail. The consultant midwife’s role is to provide evidence-based information, find out what matters to you, and discuss your options. At Kingston we are committed to supporting your decisions.
If you plan a caesarean, can you choose the date?
If you decide to plan a caesarean, you will usually be offered a date around 39 weeks of pregnancy. Babies born by caesarean earlier than this are more likely to need admission to the neonatal unit for help with their breathing: 42 babies out of 1000 at 38 weeks and 18 babies out of 1000 at 39 weeks.
Around 90 out of 100 women will have their caesarean on the planned date. 10 women will go into labour earlier and have a caesarean sooner than planned. Occasionally, if labour progresses quickly, it is safest to have a vaginal birth. The date may also change because of unforeseen situations on the day of your operation. If this happens, your healthcare team will arrange a new date with you as soon as possible.
What are the chances of any complications?
To help decide what option is best for you, you may want to consider the risk of complications with each type of birth.
|
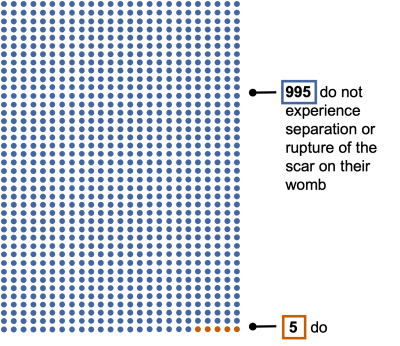
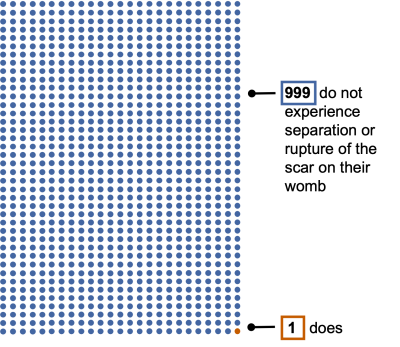
How many women experience separation or rupture of the scar on their womb? If this happens, an emergency caesarean is recommended. Serious consequences for you or your baby are rare. |
|
VBAC |
Planned caesarean |
|
|
 |
|
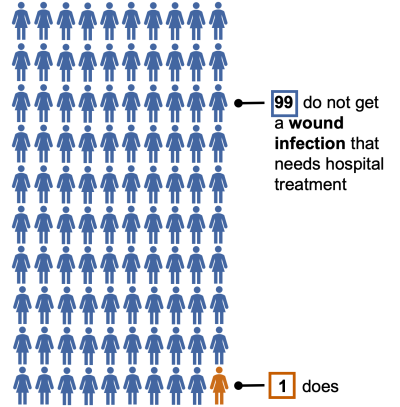
How many women get a wound infection and need to be admitted to hospital for treatment? |
|
|
|
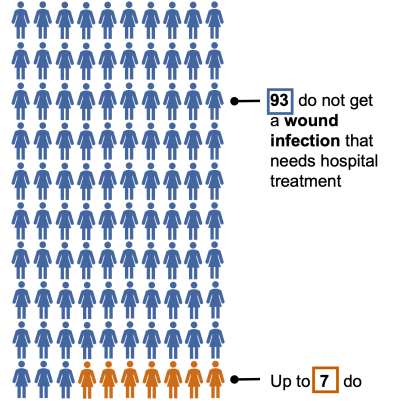 |
|
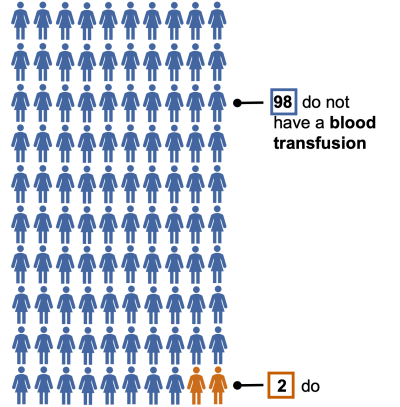
How many women have a blood transfusion? |
|
|
|
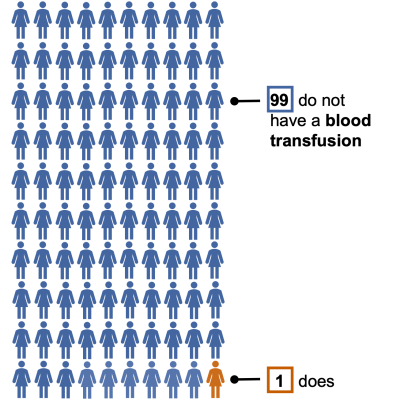 |
|
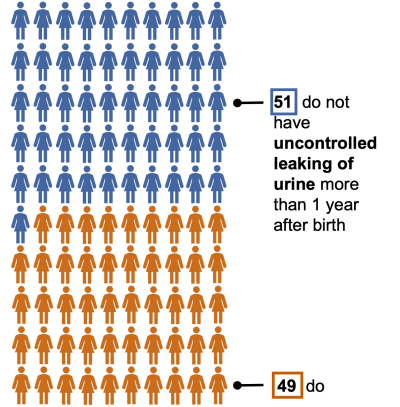
How many women have some uncontrolled leaking of urine more than 1 year after birth? |
|
|
|
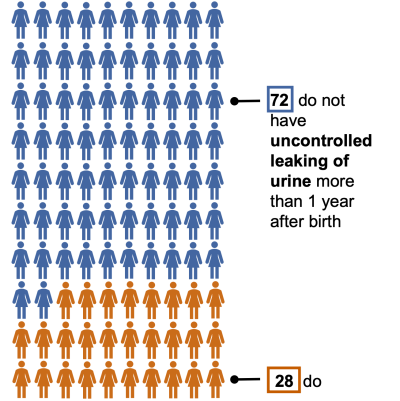 |
|
How likely are other complications? |
|
|
If you have a straightforward vaginal birth, the chance of serious complications (such as heavy bleeding) is low. If you have an assisted vaginal birth (forceps or ventouse) you are more likely to have a significant perineal tear. About 1-12 out of a 100 women are affected. If you have an unplanned caesarean, the risk of complications is higher compared to a planned caesarean. |
Repeated caesareans increase the chance of scar tissue causing organs in the abdomen to stick together (adhesions). This makes any future surgery more complex and increases the chance of bladder or bowel damage. Repeated caesareans increase the chance of conditions where the placenta attaches or grows incorrectly. These conditions increase the likelihood of significant blood loss at birth and sometimes an emergency hysterectomy (an operation to remove the womb). These conditions are more likely after multiple caesareans. |
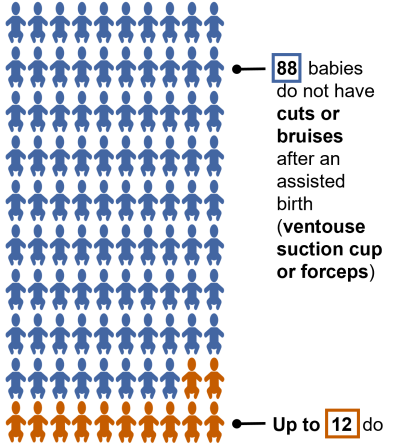
| How many babies have a minor skin injury, such as a bruise or cut? | |
|
If you have a straightforward vaginal birth, it is unlikely your baby will have any cuts or bruises. After a forceps birth, up to 10 out of 100 babies have small temporary marks on their face or head. After a ventouse (suction cup) birth, up to 12 out of 100 babies will have a temporary bruise or swelling on the head.
|
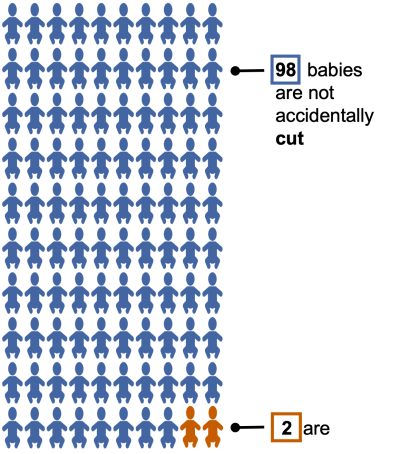
Up to 2 out of 100 babies may be accidentally cut during a caesarean. This usually heals without any further harm.
|
| How many babies have a serious injury caused by a lack of oxygen during the birth? | |
|
Out of 10,000 babies, 8 have a serious brain injury due to a lack of oxygen at birth; 9,992 babies do not. |
Out of 10,000 babies, less than 1 has a serious brain injury due to a lack of oxygen at birth; 9,999 babies do not. |
What’s next?
You will be offered an appointment to discuss your options. You can change your mind at any point in your pregnancy. Visit our website to hear women talk about their experiences of VBAC and caesarean birth.
Text-only summary of statistics above, for those who use assistive technology
If you plan a VBAC, what are the chances of a vaginal birth? |
Out of 100 women choosing VBAC, with a straightforward pregnancy who go into labour naturally, how many have a vaginal birth?
|
If a woman has also previously had a vaginal birth, the numbers are even higher:
|
What are the chances of any complications? |
|
How many women experience separation or rupture of the scar on their womb?
|
|
How many women get a wound infection and need to be admitted to hospital for treatment?
|
|
How many women have a blood transfusion?
|
|
How many women have some uncontrolled leaking of urine more than 1 year after birth?
|
|
How likely are other complications? VBAC:
Planned caesarean: Repeated caesareans increase the chance of scar tissue causing organs in the abdomen to stick together (adhesions). This makes any future surgery more complex and increases the chance of bladder or bowel damage. |
|
How many babies have minor skin injury, such as a bruise or cut? VBAC:
Planned caesarean:
|
|
How many babies have a serious brain injury caused by a lack of oxygen during the birth?
|
Contact information
Antenatal appointments
Telephone:
020 8934 2290
(Monday to Friday, 8.30 am to 4.30 pm)