Neurodiversity information for parents and young people
About biliary drainage
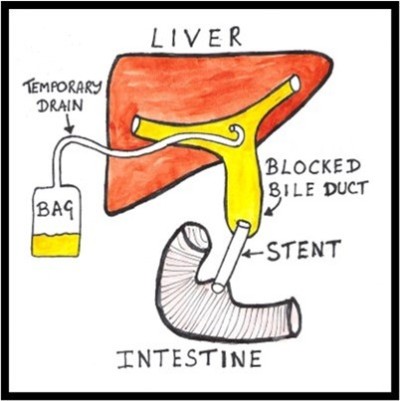
Your liver is a vital organ that cleans your blood, passing waste products into a liquid called bile. Normally this bile flows out of your liver through a tube called the bile duct, draining into your intestine.
Percutaneous biliary drainage is a way of relieving the pressure on your liver, without you needing an operation. Percutaneous means 'through the skin' and biliary means 'from your bile duct'.
We use pictures from an ultrasound scanner and an X ray machine to guide a thin plastic tube through your skin, into your liver, to drain the buildup of bile to the outside.
About biliary stents
Once we have successfully inserted the biliary drainage tube, the pressure in your liver will be relieved and bile will start to drain into the external bag.
This diverts the buildup of bile to the outside and leaves you with a plastic tube protruding from your skin. Usually, we then insert a second tube inside your body between your liver and intestine. This tube is called a biliary stent, which is a spring like metal sleeve. It bypasses the original blockage and allows us to remove the external drainage tube.
We generally insert this stent as a separate procedure, approximately 48 hours after the initial biliary drainage. If your biliary drain insertion is straightforward and circumstances are favourable, we can insert the stent at the same time. The stent is introduced through the same route as the drain, so there is no need to create a new hole in your skin.
Why you need biliary drainage
A previous test shows that your bile duct is blocked. This puts pressure on your liver and prevents it from working properly. Also, because your bile is no longer flowing freely, it can become stagnant and infected, putting you at risk of septicaemia (blood poisoning).
There are many reasons why your bile duct may be blocked, but whatever the cause, it is important to relieve the pressure promptly. This will allow your liver to recover function and drain any infection that may be developing.
An attempt may already have been made to unblock the bile duct with an ERCP (using a fibre optic telescope through the mouth). If this is unsuccessful, we usually try a biliary drainage next.
Your consultant and your interventional radiologist feel that this is the best treatment option for you. They will discuss their recommendation with you and they will take your opinion into account. You will have the chance to ask questions. If, after discussion with your doctors, you do not want us to carry out the procedure, you can decide against it.
We will only go ahead with this procedure after you have given us your written consent.
Who performs the procedure and where it takes place
An interventional radiologist will perform the procedure. This is a doctor who specialises in performing percutaneous (through the skin) procedures under ultrasound and X ray control.
The procedure will normally take place in the Interventional Screening Room which is part of the Kingston Hospital Radiology Department. If a patient is too ill to be moved, we can perform the procedure at the hospital bedside using portable equipment.
Preparing for your procedure
[Amanda: Is this usually inpatient or outpatient or both?]
To prepare for the procedure do the following.
- You can take sips of water up to 2 hours before the procedure.
- You can take your normal medicines up until the procedure.
- Tell your doctor [Amanda, other leaflets say ‘Tell the Interventional Radiology Unit’] if you have previously had allergies to foods, medicines or intravenous contrast medium (the dye used for kidney X rays and CT scans).
- Tell your doctor [Amanda, other leaflets say ‘Tell the Interventional Radiology Unit’] if you have been on blood thinning tablets such as warfarin, aspirin or clopidogrel.
- We will give you some pre procedural painkillers and antibiotics if you need them.
When you arrive in the department, you will meet the team, including your nurse, interventional radiologist and radiographer. The radiographer operates the equipment and is responsible for the images we obtain.
- We will ask you to lie on the X ray table, on your back.
- You will already have an intravenous cannula (a small flexible tube) inserted on the ward prior to the procedure. This is so we can give you antibiotics, painkillers or sedation directly into your blood.
- We will wrap a cuff around your arm to monitor your blood pressure. We will place a clip on your finger to measure your pulse and breathing.
- The doctor performing the procedure will choose the most appropriate point on your skin, clean this area with antiseptic and anaesthetise it with an injection.
- We will guide a fine needle through this numb area, into your liver and bile duct using the pictures from the scanner and X ray machine.
- Using a guidewire, we will exchange the needle for a plastic tube which we will connect to a bag. We will secure it with some stitches and cover it with dressings.
Pain
After we administer pain killers and inject you with local anaesthetic, your skin and deeper tissues will go numb.
Everyone experiences pain differently and some people will find the procedure painful. If you do feel any pain, the nurse looking after you can arrange stronger pain relief and sedation.
How long it takes
Each case is individual but you can expect to be in the department for approximately 2 hours. Much of this time is spent in preparation and considerably less time is spent inserting the tube itself.
Looking after your drainage tube
Your drainage tube is important for your recovery
Your nurse will check the bag regularly, to monitor how much fluid is draining and to prevent the bag becoming too heavy.
- Avoid pulling the tube out by accident while it remains in place.
- Avoid sudden movements.
- Always make sure that the attached bag can move freely with you.
- Avoid getting the tube twisted or pulled.
- Let your nurse know immediately if you think the tube has been pulled in any way.
What happens next
We will give you an X ray approximately 48 hours after we insert your stent. This will check that the stent is working properly and in a good position.
If everything looks satisfactory, we can remove the external drain, leaving just the stent inside.
The stent does not specifically treat the underlying blockage; it only bypasses it.
It will allow time for us to further assess the cause of the blockage and plan treatment for you.
Risks
It is likely that you have either had an unsuccessful ERCP procedure (using a fibreoptic telescope through the mouth) or that an ERCP was not considered appropriate for you.
Percutaneous biliary drain and stent insertions are general safe procedures. However, a few serious risks or complications can arise, as follows.
- Damage can occur to nearby bodily structures. This rarely causes a serious problem.
- Bleeding can develop. This rarely causes a serious problem.
- If your blocked bile duct is infected, some infection can spread into your blood stream and give you a shivering attack and blood poisoning. We give you antibiotics directly into your blood to protect against this.
- Sometimes we are not able to place the stent correctly.
- Sometimes, even if we place the stent correctly, it may block and fail to work. In this situation you may require an operation.
If you have concerns or questions about this procedure, you can discuss these with your medical team and your interventional radiologist at any time.
Contact information
Interventional Radiology Unit
Interventional Radiology Unit Charge Nurse
Telephone:
Interventional Radiology Unit: 020 8934 6206
Interventional Radiology Unit Charge Nurse: 020 8934 2758