Neurodiversity information for parents and young people
About angioplasty
Angioplasty is a form of ‘pin hole’ surgery which allows artery blockages to be stretched open with a balloon, improving blood flow and reducing symptoms.
We usually perform it via a small incision (cut) in your groin, while you are under local anaesthetic.
Not all blockages are suitable for treatment with angioplasty. In most cases, an angioplasty can avoid the need for a conventional operation, which is safe but carries slightly higher risks due to its complexity.
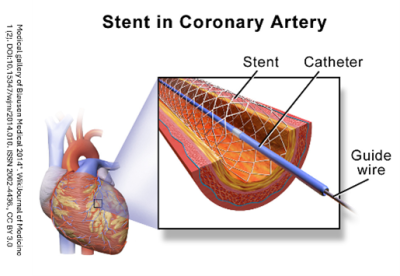
About stents
A stent is a spring like metal sleeve that we insert across an arterial blockage. We then release it to hold the artery wide open. We can use a stent if angioplasty alone fails to improve your blood flow sufficiently.
Why you need an angioplasty and stent
Your symptoms are being caused by one or more blocked arteries. Blockages reduce the flow of blood and starve your muscles and tissues of the oxygen and nutrients they need.
Your doctor and interventional radiologist feel this is the best treatment option for you. They will discuss their recommendation with you, and they will take your opinion into account. You will have the chance to ask questions. If, after discussion with your doctors, you do not want us to carry out the procedure, you can decide against it.
We will only go ahead with this procedure after you have given us your written consent.
Who performs the procedure and where it takes place
An interventional radiologist will perform your angioplasty. This is a doctor who specialises in performing percutaneous (through the skin) procedures under imaging guidance. They have expertise in using X ray and scanning equipment and in interpreting the images it produces. They use these images on screen, to guide the procedure.
We will perform the procedure in the Interventional Screening Room, part of the Kingston Hospital Radiology Department.
Preparing for your procedure
You need to be an inpatient in the hospital, even if it is only for the day.
- You can take sips of water up to 2 hours before the procedure.
- You can take your normal medicines up until the procedure.
- When you receive your appointment letter, tell the Interventional Radiology Unit if you have previously had allergies to foods, medicines or intravenous contrast medium (the dye used for kidney X rays and CT scans).
- When you receive your appointment letter, tell the Interventional Radiology Unit if you have been on blood thinning tablets such as warfarin, aspirin or clopidogrel.
When you arrive in the department, you will meet the team, including your nurse, interventional radiologist and radiographer. The radiographer operates the equipment and is responsible for the images we obtain.
- We will ask you to lie on the X ray table.
- We will place an intravenous cannula (a small flexible tube) in a vein on your arm to give you sedation or other required medicine.
- We will wrap a cuff around your arm to monitor your blood pressure, and place a clip on your finger to measure your pulse and breathing.
- We will clean a patch of skin and anaesthetise it, usually over your groin.
- Through this numb patch, the radiologist will advance a needle into your artery and, using a guidewire, exchange it for a thin plastic tube called a catheter. With the catheter in place, we will inject X ray dye to allow us to take pictures of your arteries.
- The X ray dye can cause a warm, glowing feeling but this passes quickly and is not painful.
- We will treat any suitable blockages with angioplasty or stenting and take follow up pictures at the same time, to check the result.
- Once the radiologist is satisfied, we will remove the catheter and the radiologist will press firmly on the skin entry point for several minutes, to prevent any bleeding.
Pain
When we inject the local anaesthetic, it will sting to start with, but this wears off after about 20 seconds. Your skin and deeper tissues will feel numb and the procedure is unlikely to be painful.
If you do experience any further discomfort, the nurse looking after you can arrange some stronger pain relief and sedation through the cannula in your arm.
How long it takes
Every patient's situation is different. As a guide, you can expect to be in the Radiology Department for about 2 hours.
After the procedure
After the procedure, we will take you back to the ward. Nurses on the ward will carry out routine observations, such as taking your pulse and blood pressure. They will also look at the skin entry point to make sure there is no bleeding.
The standard procedure is for you to stay in bed for 6 hours, to allow the hole in your artery to mend so that it is safe for you to get up and walk. Patients usually stay in hospital overnight and we discharge them the following morning.
Risks
Angioplasty is a safe procedure, but risks and complications can arise. These include the following.
- Bleeding at the needle insertion site which may result in a small bruise called a haematoma.
- If bleeding is persistent or if the angioplasty balloon and catheters have damaged the artery, the patient will require an urgent operation to stabilise the situation. This is rare.
- There can be harmful or allergic reactions to the X ray dye and other medicines. These are rare.
We will identify your risk factors during your pre procedure assessment, and take suitable precautions. We will closely monitor your during the procedure and the staff looking after you will be ready and equipped to treat reactions if they arise.
If you have concerns or questions about this procedure, you can discuss these with your medical team and your interventional radiologist at any time.
Contact information
Interventional Radiology Unit
Interventional Radiology Unit Charge Nurse
Vascular Surgical Unit, Pre-Assessment Nursing Sister
Telephone:
Interventional Radiology Unit: 020 8934 6206
Interventional Radiology Unit Charge Nurse: 020 8934 2758
Vascular Surgical Unit, Pre-Assessment Nursing Sister: 020 8934 3668